Cancer Pain and Opioid Use Disorder
Investigators support individualized approaches and compassionate care to minimize nonmedical opioid use and opioid use disorder in patients with cancer pain.
ABSTRACT
Opioid use disorder (OUD) is increasingly recognized and co-present in patients with cancer. Unfortunately, OUD is not addressed or treated adequately in oncology settings. In addition, patients with cancer-related pain treated with narcotic pain medications are at risk for nonmedical opioid use (NMOU). More than two-thirds of patients with advanced cancer have pain. Both OUD and NMOU need to be concomitantly addressed alongside cancer-related pain management to avoid complications such as overdose. We review the approach to identifying and treating OUD and NMOU in patients with cancer and cancer-related pain.
Oncology (Williston Park). 2022;36(9):535-541.
DOI: 10.46883/2022.25920973
Introduction
Primum non nocere. It is troubling to think that the medications, opioids specifically, meant to alleviate pain and suffering may inadvertently cause more harm than good. However, the harms caused by inappropriate opioid prescribing have been well documented in the noncancer population and help guide opioid prescribing in patients with cancer.1 Of the cardinal ethical principles of medical care, respect for nonmaleficence can be particularly challenging when the vehicle of providing symptomatic relief for many patients carries the burden of addiction for some. On a national scale, responses to the opioid epidemic recapitulate similar anxieties about managing pain in the face of substance use disorders.2
Pain is highly prevalent in all patients with cancer (30%-50%); its presence is especially relevant for patients with advanced cancer (approximately 70%) managed primarily by medical oncologists.3 Given the high lifetime prevalence of substance use disorders, many patients who develop cancer will have a preexisting opioid use disorder (OUD), and many more patients will be prone to nonmedical opioid use (NMOU) and other forms of what has been termed chemical coping.4,5 Nonmedical opioid use encompasses a broad spectrum of nonprescribed opioid use that is particularly relevant for patients with cancer who also experience pain. The definition comes from the US National Survey on Drug Use and Health and includes use of opioids without a prescription, use with a prescription but not as prescribed, or use intended primarily for the purposes of the experience of feeling caused by opioids.6 Consistent with the increasing prevalence of OUD in the general population, an increase in opioid-associated deaths was observed in patients with cancer specifically from 2006 to 2016.7 In addition, patients may develop OUD during or after their treatment for cancer. Therefore, screening, assessments, and discussions about substance use should be routine and its management seamless given the logistical nuances of cancer care.5
The co-emergence of cancer and OUD develops from (1) patients with a history of OUD or other substance use disorders who develop cancer or (2) patients with cancer who develop OUD. The latter group originates from the iatrogenic development of OUD. Unfortunately, the iatrogenic contribution of opioid exposure to OUD and its etiology are not well understood.8 Although iatrogenic development of OUD represents the minority of OUD, it certainly warrants further research. Even still, many patients taking opioids will not belong to either group but may be at high risk for NMOU, especially given the high prevalence of psychosocial stressors in patients with cancer.
Herein we review strategies for the management of pain in patients with cancer and concomitant OUD, either preexisting or developing while being treated for pain, and strategies for pain management in patients with cancer who are at high risk for NMOU.
Methods
We performed comprehensive searches of PubMed and Google Scholar for all relevant publications about OUD, more specifically in patients with cancer pain, using the following keywords: oncology, cancer, opioid, opioid crisis, pain, palliation, opioid misuse, dependence, opioid use disorder. We focused primarily on the studies that described oncological pain along with opioid use and current pharmacologic therapies to manage OUD. We excluded abstracts, comments, and non–English language articles.
Screening for Aberrant Opioid Use
Clinical practice guideline recommendations for active screening and monitoring of opioid pain management are conspicuously incomplete despite the importance of opioids to treat cancer pain and the risk of aberrant use.5 A descriptive study of pain management practices found that clinicians were less likely to use urine toxicology screening while prescribing opioids or refuse opioid prescriptions for patients with cancer vs noncancer patients.9 The National Comprehensive Cancer Network (NCCN) recommends the use of Risk Evaluation and Mitigation Strategy tools that have been put in place and are FDA approved for individual opioid products.10 The NCCN recommends using state-run prescription drug monitoring programs and that clinicians are educated on aberrant use behaviors.10 Briefly, these include such behaviors as compulsive use and preoccupation, overt cravings, and loss of control, as well as continued use despite harm.11 In addition to patient education regarding opioid products and evaluating therapeutic response to opioids, the NCCN also recommends evaluating patients for risk factors associated with opioid misuse/abuse/diversion and monitoring for opioid misuse and abuse. Screening tools are available for this purpose but are not specific to cancer-related pain management.12 A history of illicit drug, alcohol, or substance dependence, in addition to a family history of substance abuse, indicates higher risk of aberrant opioid use. In addition, younger patients with a history of legal problems, incarceration, or psychiatric disorders such as posttraumatic stress disorder, bipolar disorder, anxiety, and depression have an increased risk of aberrant opioid medication use.12 The NCCN guideline recommendations encourage patients with a history of addiction to be treated for cancer-related pain in coordination with an addiction specialist. In addition, patients with high-risk factors for opioid misuse benefit from psychosocial education, support services, and cognitive behavior therapies that address problem-solving techniques and strategies to reduce the impact of modifiable risk factors.10 Clinicians should consider interdisciplinary collaborations, including early referrals to interventional pain specialists, to maximize the use of nonopioid strategies for pain relief. Outpatient visits should be frequent, such as weekly, if possible, to reduce the quantity of prescribed opioids at any given time point.
Evaluation of Psychosocial Stressors
A global symptoms assessment is imperative for comprehensive pain management because depression, anxiety, and psychological distress worsen the severity, tolerability, and chronicity of perceived pain. At the same time, to be in pain is to be distressed, which may precipitate or worsen anxiety and depression. Also, depression lowers pain tolerance.13 Complications, including changes in patterns of sleep, cognition, personality, or other substance use disorders, are both causes and consequences in this circular process that characterizes what has been termed total pain by palliative care founder Dame Cicely Saunders.14-16 The purpose of structured symptom assessments is to untangle the bidirectional relationship between painful conditions and mental health and identify areas of dysfunction where intervention may decrease suffering.
Adequate management of OUD, in addition to cancer-related pain, requires appropriate attention to the constellation of concomitant neuropsychiatric symptoms (eg, depression, anxiety, insomnia, cognitive impairment) that often accompany pain. The American Society of Clinical Oncology and the NCCN have put forth guideline recommendations for screening and treatment of these symptoms.10,17 Although concomitant psychiatric symptoms may abate while adequately addressing pain, it is generally recommended both are treated concomitantly. Psychoeducation plays a role in helping patients understand the relationships among pain, depression, insomnia, and poor executive function, for example. Patients should have an idea of when they are experiencing anxiety, for example, in the setting of pain or by itself, to facilitate the administration of as-needed medications. In addition, clinicians who treat cancer-related pain, especially in the setting of OUD, should be able to readily recognize affective disorders (eg, depression, anxiety) and cognitive disorders (eg, delirium). Diagnostic uncertainty and treatment trepidation should be met with prompt referral to mental health clinicians and symptom specialists. Comprehensive screening tools can expedite recognition and treatment of these concomitant symptom clusters.
Psychosocial screeners and multisymptom assessment tools should be collected concomitantly with opioid risk assessment tools, such as the Opioid Risk Tool or the Screener Opioid Assessment for Patients with Pain.18,19 Psychological distress, anxiety, and depression could be assessed using the Distress Thermometer and Problem List, the Edmonton Symptom Assessment Scale, or PROMIS (Patient-Reported Outcomes Measurement Information System) measures. PROMIS measures can be used to assess many psychosocial symptoms. They are derived from legacy measures and are validated in cancer settings. Insomnia may be addressed by questioning sleep hygiene habits and assessing for initial, middle, and terminal insomnia patterns. Cognitive impairment and delirium should be assessed by multiple time point assessments of awareness, orientation, and attention. Several brief self-report and clinician-administered scales measure attention and evaluate for cognitive impairment. The assessment of alcohol and other substance use disorders may be accomplished using PROMIS measures, and the CAGE (cut down, annoyed, guilty, eye-opener) screener for alcohol use may be extended to include substance use.20 In addition, well-performing abbreviated and single-item screeners are available for alcohol (Alcohol Use Disorders Identification Test Consumption)21 and other drug22 use, which can trigger further screening with the full Alcohol Use Disorders Identification Test or referral to treatment.
Case Presentation
A 57-year-old man is being treated for recurrent small cell lung cancer with third-line chemotherapy. He notes increasing bony pain requiring escalating doses of short-acting hydromorphone in addition to the extended-release morphine formulation he is already taking. In addition to pain from bony metastasis, he has various psychological concerns, such as anxiety (likely precipitated by shortness of breath), initial and terminal insomnia, fatigue, and memory impairment. His clinicians have become frustrated with what seems to be inconsistent and excessive use of as-needed short-acting hydromorphone as he admitted taking more than prescribed to help with sleep and anxiety.
The patient has no personal or family history of drug use or alcoholism. He denies other significant psychosocial stressors aside from having lung cancer. Universal screening reveals the presence of partially treated pain, no evidence of cognitive impairment or delirium, a positive urine drug screen for opioids, and the presence of severe insomnia, anxiety, and depressive symptoms.
Nonmedical Opioid Use
The National Institute on Drug Abuse defines NMOU as “taking an opioid in a manner or dose other than prescribed, taking someone else’s prescription opioid, even if for a legitimate medical reason, or taking prescription opioids for the feelings that it produces.”23 Chemical coping and NMOU are related concepts. Chemical coping refers to the use of opioid medications to treat psychological suffering or emotional distress.24 It is a controversial term that was first used to described drug-seeking behaviors of patients with end-stage alcoholism.25 This nomenclature may be experienced as stigmatizing, and, therefore, it may be more helpful and appropriate to address unresolved distress. Of course, pain is intimately related to psychological distress. Pain relief may alleviate distress; therefore, patients may use opioids in excess of what is needed to treat pain if distress is also ameliorated vis-à-vis opioid medication. Education regarding appropriate use of opioids and adequate screening for psychological comorbidities are key principles for addressing NMOU and chemical coping. Nonmedical opioid use may occur as a form of chemical coping or opioid use for other non–pain-related reasons. It may result from opioid availability and lack of mental health resource or psychoeducation availability, and the presence of mental health stigma. Oversight of NMOU and chemical coping requires not only limiting opioid medication availability but also providing needed psychoeducation, screening and triaging for psychosocial distress, and making nonstigmatizing mental health referrals. In fact, assessing for NMOU is an opportunity to assess psychosocial distress as well.
The problem with NMOU is the inappropriate use of potentially dangerous and addictive medication to suboptimally treat psychological symptoms. Anxiety, depression, and insomnia are more safely and effectively treated with appropriate (non)psychopharmacologic agents to target those symptoms. This syndrome is more common among young, male patients with a history of alcohol use, drug use, and smoking.26,27 Patients who rapidly escalate the opioid dose, frequently complain of pain with intensity of 10 of 10, or are at risk for chemical coping should be referred to a supportive care/palliative care team for interdisciplinary management usually consisting of a pain management specialist and counselors. Addressing the most pertinent issue should help limit chemical coping and NMOU. At other times, patients will have a known history of OUD, which may be uncovered or develop while dealing with the stresses of cancer. By definition, patients with OUD are at high risk for losing control of their opioid use and will have higher rates of other psychosocial factors that generally make pain more severe, and they tend to be more intolerant of pain (this abates to some extent when they are treated for OUD), requiring higher doses of opioids for pain control. Patients with OUD should be treated for OUD while receiving treatment for cancer-related pain.28
In the case presentation, it is likely that NMOU would abate with psychoeducation and adequately addressing anxiety, depression, and insomnia.
Opioid Use Disorder
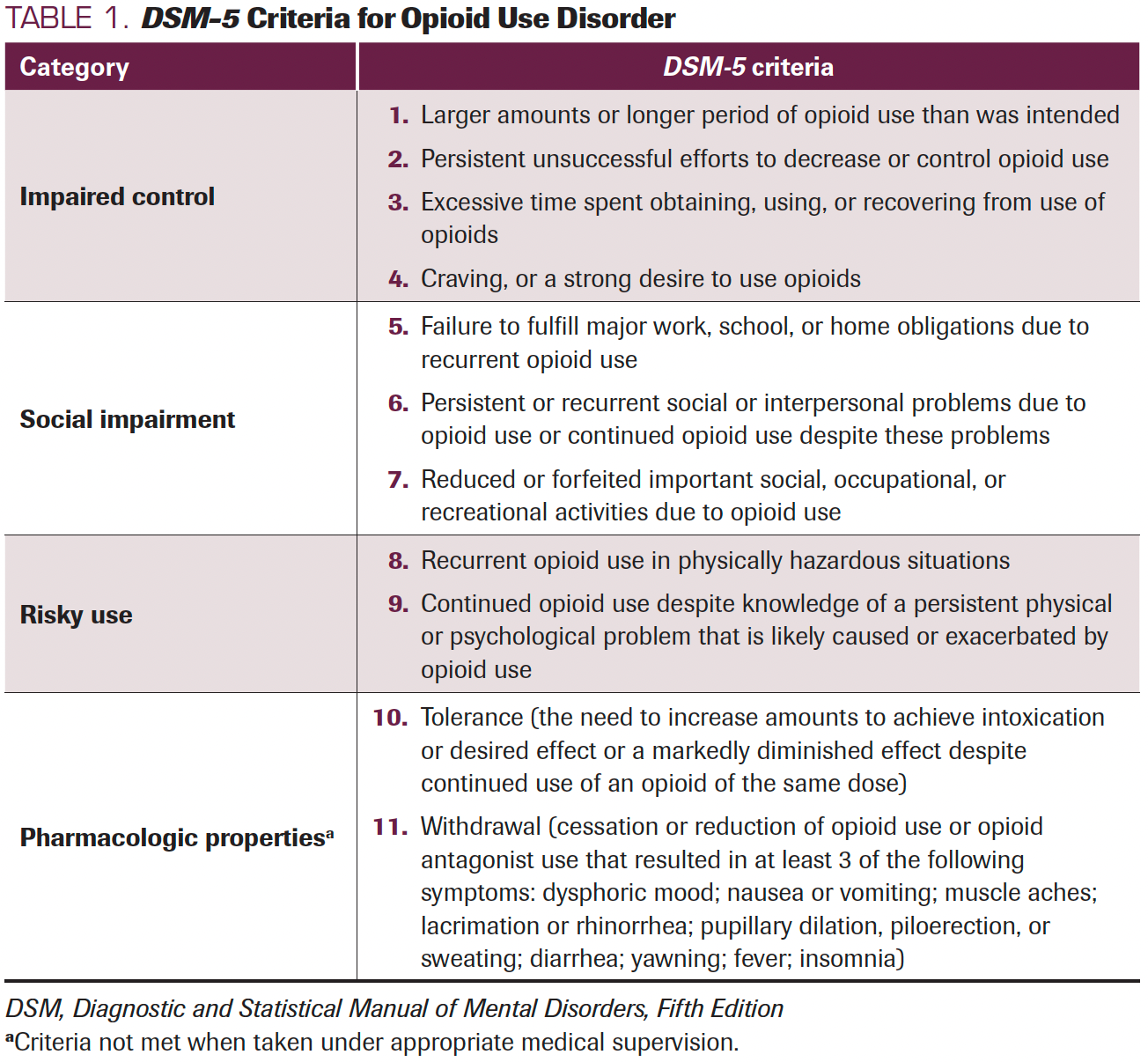
A person is defined as having an OUD when there is a pathologic pattern of behaviors related to opioid use, which is a combination of cognitive, behavioral, and physiologic symptoms.29 The person continues substance use despite emerging substance-related problems, which causes significant impairment or distress. The full diagnostic criteria are given in Table 1. A patient must meet at least 2 diagnostic criteria, and severity is stratified as mild, moderate, or severe if they meet 2 or 3, 4 or 5, or more than 6, respectively. A limitation of these diagnostic criteria is that severity is based on frequency of criteria rather than on impairment. A person could meet 7 criteria (severe) yet have little functional impairment, and someone else could meet 3 criteria (mild) and have significant functional impairment.
TABLE 1. DSM-5 Criteria for Opioid Use Disorder
Tolerance or withdrawal (often termed physiologic dependence) may occur during the appropriate use of opioid therapies and should not be counted toward a diagnosis of OUD when opioids are used solely under appropriate medical supervision. Because many clinicians and patients are concerned with the possibility of opioid dependence, this is a key distinction that is diagnostically relevant. Furthermore, many patients exhibit signs of pseudoaddiction, a term coined in 1989 by Weissman and Haddox30 to describe an “iatrogenic syndrome that mimics the behavioral symptoms of addiction” in patients with inadequate pain control. Although the existence of pseudoaddiction, as defined, is controversial, the concept remains present in the medical literature and seems to highlight a clinically relevant concept. These patients are usually identified by notable behaviors such as demanding specific opioids to treat their pain or other classic signs of drug-seeking behavior, but these behaviors should cease once adequate pain control is achieved. Therefore, patterns of drug use, including route of administration (intravenous or intranasal), frequency, impairment (ie, social, personal, professional), and other substance use should be explored.
A complete history with necessary collateral information is needed to entertain a diagnosis of OUD: a physical examination in addition to full social and mental health histories should be acquired from the patient.31 The physical examination may reveal a patient in intoxication (confusion, miosis, hypersomnia, nausea, euphoria, constipation, decreased pain perception) or withdrawal. Urine drug tests are necessary during initial and follow-up visits to ascertain the type of opioid substance used and other comorbid substance use, as well as to monitor remission and maintenance.32 In most areas it is now necessary to include urine testing for fentanyl, which is often not included in standard urine drug test batteries.33 If the patient has a history of intravenous drug use, tests such as infectious screening (HIV, hepatitis B, hepatitis C) are recommended; echocardiography to rule out endocarditis should be ordered for those with a history of bacteremia.31
Complex persistent opioid dependence (CPOD) can develop from long-term opioid dependence and shares many features with OUD, including the biological mechanisms associated with UOD. Complex persistent opioid dependence develops in the setting of opioid therapy that has not been effective but does not meet the criteria for OUD. It exists on a continuum between simple physical dependence and OUD. Complex persistent opioid dependence should be considered when long-term opioid use and tapering are not effective. Interestingly, CPOD may respond to buprenorphine treatment, which can also be used in a chronic pain setting. Delineating the diagnostic entity associated with dysfunctional or inappropriate opioid use has underlying treatment implications. Universally, psychosocial factors, along with nonpharmacologic management of pain, should be considered in all cancer-related pain treatment plans.
Management of Opioid Therapies in Patients With Cancer Who Have OUD
Given that approximately one-half of patients with cancer were prescribed an opioid during the year of their initial diagnosis, safe and effective pain management needs to be achieved while considering the management of OUD. Although the focus of this review is safe opioid prescribing in patients with OUD, one might consider the phenomenon of opioid misuse as a continuum, with chemical coping, NMOU, or CPOD being an early stage of substance use disorders.34,35 In the early stages when patients use opioids to treat anxiety, depression, or sleep disorders, these actions can often be countered with compassionate use of motivational interviewing to assist them in gaining insight into their behaviors and to appropriately treat their emotional distress. Early identification is necessary.35,36 The cancer setting (eg, type, stage) and whether the patient is being treated with curative intent play a role in prediction of ongoing pain and concomitant neuropsychiatric symptoms. Although early identification of pain, along with adequate treatment strategies, are still paramount, the concomitant considerations vary based on treatment setting. In the curative setting, the clinician may be most worried about addressing cancer-related pain and OUD to facilitate adherence with anticancer treatments, whereas quality of life and symptom management may be further prioritized in the palliative setting.
In addition, nonpharmacologic measures should be instituted just as would be appropriate for a patient with cancer but without OUD. These modalities include psychoeducation regarding activity and addressing pain management strategies proactively, exercise therapy as tolerated, mindfulness and stress reduction, group support activities, spinal manipulation, acupuncture, yoga, and other multimodal integrative therapies, as well as nonopioid analgesics such as nonsteroidal anti-inflammatory drugs, selected anticonvulsants (eg, gabapentin and pregabalin), and selected antidepressants (eg, duloxetine for peripheral neuropathy, amitriptyline for insomnia and irritable bowel syndrome types of pain).37-39 Despite the widespread use of medical marijuana in patients with cancer and its potential use in addressing OUD, the evidence base is lacking, and, therefore, medical marijuana cannot be recommended to offset opioid-based medications for OUD (MOUDs).40,41
Patients with ongoing, untreated substance use disorders require more complex care than can usually be provided in an oncology setting without significant interdisciplinary support.42 The goal may be the provision of pain control while using “harm reduction,” which means the highest level of safe and effective care. The priorities of the harm reduction model of care for OUD are prevention of overdose and other consequences of unsafe use (eg, accidents, infections), increased control over use (ie, decreasing the total amount used), and preventing diversion.43 A week’s supply of opioid may be prescribed, rather than 1 month, and frequent urine screening may be used. Interdisciplinary care is warranted. Furthermore, people with a medical history of substance use disorder and those who are in recovery may present a unique challenge. Fears of relapse when presented with an opioid for the treatment of cancer pain may lead the patient to refuse these medications. Available evidence does not support an increased risk of relapse for patients treated with opioid analgesics who are maintained on medications for OUD.44-46 Having thoughtful discussions about use of opioids, trying nonopioid analgesics, using interventional therapies, and incorporating the patient’s sponsor or case manager can help provide effective relief while limiting the risk of relapse.
Currently, there are 2 evidence-based MOUDs: buprenorphine and methadone, which are also approved for pain.47,48 Buprenorphine acts as a partial mu receptor agonist with high affinity and slow dissociation and may precipitate withdrawal as it may displace other opioids. It is combined with naloxone in most formulations approved for OUD, to prevent inhalation or injection use of the products. Methadone is a full mu receptor agonist with a long half-life. Both medications blunt euphoria, decrease craving, and are medically safe. They reduce risk of overdose, acute and chronic infections, and suicide.49,50 In general, patients with cancer have at least double the risk of suicide, but the risk becomes exceedingly pronounced with pain and the first few weeks to months after diagnosis or other cancer-related crises.51 Buprenorphine and methadone have different dosing schedules for OUD treatment and analgesia: for pain management, they are prescribed at lower doses several times daily, as opposed to once-daily dosing for OUD. Use of these medications to treat OUD is highly regulated. Buprenorphine prescribers need to receive a Drug Enforcement Agency waiver with limitations on the number of patients to be enrolled in the clinic, whereas methadone maintenance treatment must be administered in a federally approved treatment program. These restrictions do not apply to prescriptions intended to treat pain. There is a dearth of evidence regarding dual treatments for co-occurring OUD and cancer pain. Therefore, in 2021, Merlin and colleagues52 conducted an online modified Delphi approach to develop consensus for managing cancer pain in patients with OUD from experts in the discipline of hospice and palliative medicine, pain medicine, and addiction medicine. Experts agreed that nonopioid pharmacologic and nonpharmacologic treatments should be maximized before adjustments of MOUDs. The summary of the recommendation is highlighted in Table 2.
TABLE 2. Combination of Cancer Pain Management With Medications for Opioid Use Disorder
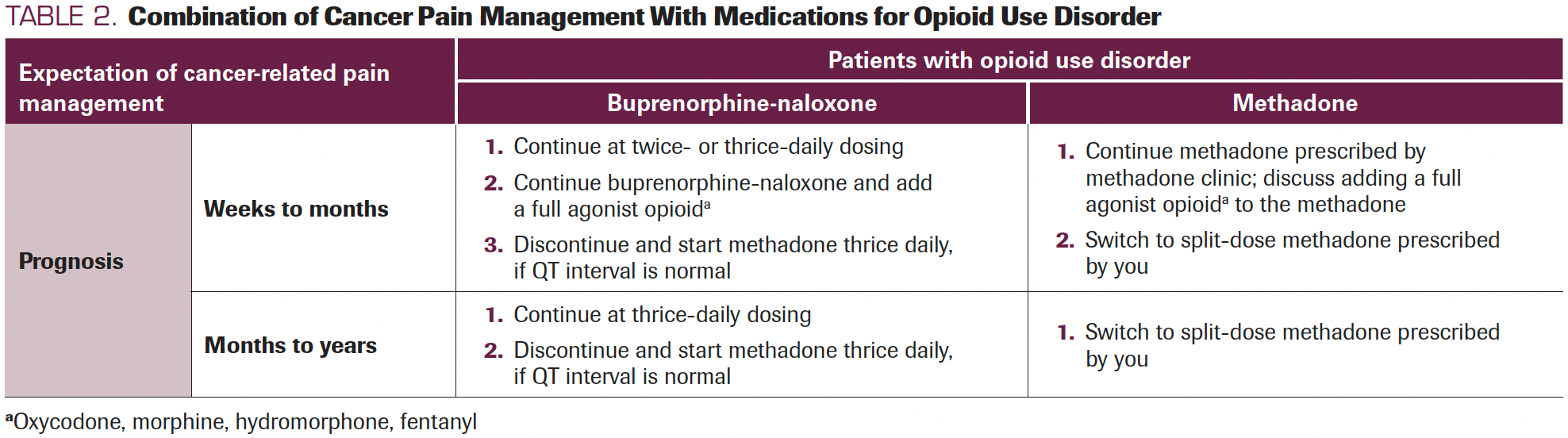
In both cases, experts agreed that it would be inappropriate to switch buprenorphine-naloxone to a methadone maintenance treatment program, and vice versa. Experts suggested switching buprenorphine-naloxone to split doses of methadone as appropriate due to perceived weaker pain control, although research by Neumann and colleagues53 has shown both medications to be equally analgesic when initiated in patients identified as being addicted to other opioids. Stopping OUD treatment completely and starting a full agonist opioid was discouraged.
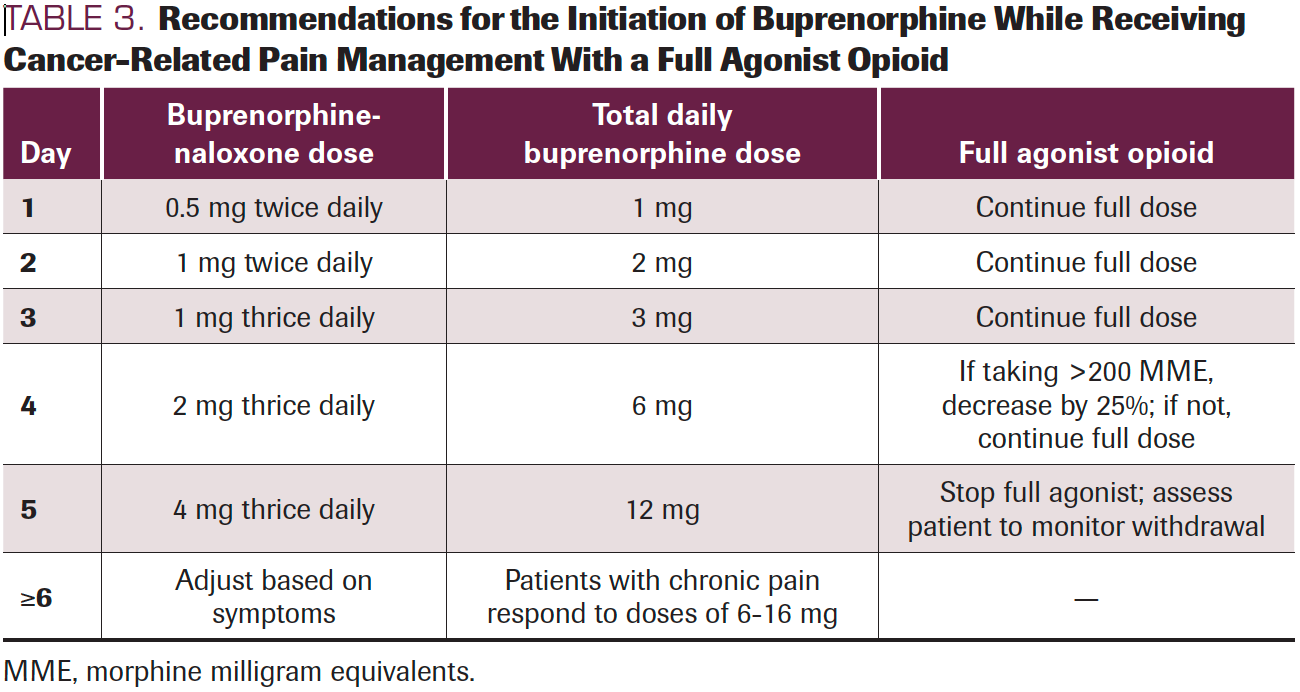
Patients who are taking a full agonist opioid to treat cancer pain but who also meet the criteria for OUD may benefit from a switch to methadone or buprenorphine as a primary analgesic therapy. Often, patients are reluctant to switch pain medications due to concerns of inadequate pain control. It is important to reassure patients that good alternatives exist, and physicians should focus on addressing the patient’s pain management while also reducing potential adverse effects from full agonist opioids and unsafe drug use. If the patient is willing to consider buprenorphine, a low-dose initiation protocol can be implemented to prevent withdrawal symptoms.54 Edens et al47,55 present their home buprenorphine initiation protocol, which has been shown to minimize adverse effects and reach therapeutic doses for both pain management and OUD by day 5 (Table 3).
TABLE 3. Recommendations for the Initiation of Buprenorphine While Receiving Cancer-Related Pain Management With a Full Agonist Opioid
Despite the recommendation that patients with OUD and cancer-related pain continue taking MOUDs, there are situations in which the clinician may need to consider also prescribing a full opioid agonist (Sidebar). For patients already established on MOUDs, mechanisms of tolerance and hyperalgesia may prevent adequate analgesia from buprenorphine or methadone alone.56 Uncontrolled pain plays a significant role in patients with OUD returning to or continuing opioid use.46 Concurrent prescribing of a short-term full agonist has been shown to reduce withdrawal and craving, address pain adequately, and prevent patients from turning to illicitly obtained opioids.57 From a harm reduction perspective, compassionate, effective care through adequate pain management minimizes the risks of unsupervised opioid use.
Conclusion
Management of cancer-related pain in patients who have OUD or are at risk for OUD requires an individualized approach based on the patient’s substance use history and pain management needs. In addition to making an accurate diagnosis of substance use disorder, a comprehensive assessment and an understanding of opioid and MOUD therapies are necessary to provide adequate patient-centered pain management. Clinicians should be aware that opioids might be misused, either inadvertently (eg, for its hypnotic and anxiolytic effects) or purposefully by those with substance use disorders; however, compassionate care and harm avoidance principles will support the cautious use of opioid medications when nonopioid and nonpharmacologic options are inadequate.
Acknowledgments:
Conflict of Interests: No conflict of interest reported by authors. We have reviewed and approved the manuscript as it is submitted and have no conflict of interest to declare. Additionally, each author met each of the authorship requirements as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. We had multiple roles in writing the manuscript including the conception, design, acquisition, analysis and interpretation of the data. The information in the manuscript has not been published previously and is not under consideration for publication elsewhere.
Author affiliations:
Amvrine Ganguly, MD1,¥; Marco Michael, MD1,¥; Simona Gorschin, MD2; Kirk Harris, MD3; and Daniel McFarland, DO2,4
¥co-first authors
1Department of Psychiatry and Behavioral Sciences, State University of New York Downstate Brooklyn
2Department of Psychiatry and Behavioral Sciences, Lenox Hill Hospital, Northwell Health, New York, NY
3Department of Psychiatry, University of Rochester, Rochester, NY
4Department of Medicine (DM), Lenox Hill Hospital, Northwell Health, New York, NY
Contact Information:
Daniel C. McFarland, DO
Department of Psychiatry and Behavioral Sciences
Lenox Hill Hospital, Northwell Health
New York, NY 10034.
Email: danielcurtismcfarland@gmail.com
References
- Humphreys K, Shover CL, Andrews CM, et al. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford-Lancet Commission. Lancet. 2022;399(10324):555-604. doi:10.1016/S0140-6736(21)02252-2
- Bates N, Bello JK, Osazuwa-Peters N, Sullivan MD, Scherrer JF. Depression and long-term prescription opioid use and opioid use disorder: implications for pain management in cancer. Curr Treat Options Oncol. 2022;23(3):348-358. doi:10.1007/s11864-022-00954-4
- van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain. 2007;132(3):312-320. doi:10.1016/j.pain.2007.08.022
- Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and treatment of opioid misuse and addiction: a review. JAMA Psychiatry. 2019;76(2):208-216. doi:10.1001/jamapsychiatry.2018.3126
- Carmichael AN, Morgan L, Del Fabbro E. Identifying and assessing the risk of opioid abuse in patients with cancer: an integrative review. Subst Abuse Rehabil. 2016;7:71-79. doi:10.2147/SAR.S85409
- Ulker E, Del Fabbro E. Best practices in the management of nonmedical opioid use in patients with cancer-related pain. Oncologist. 2020;25(3):189-196. doi:10.1634/theoncologist.2019-0540
- Chino FL, Kamal A, Chino JP. Opioid-associated deaths in patients with cancer: a population based study of the opioid epidemic over the past 10 years 2018. J Clin Oncol. 2018;36(suppl 30):230. doi:10.1200/JCO.2018.36.30_suppl.230
- Beauchamp GA, Nelson LS, Perrone J, Lyons MS. A theoretical framework and nomenclature to characterize the iatrogenic contribution of therapeutic opioid exposure to opioid induced hyperalgesia, physical dependence, and opioid use disorder. Am J Drug Alcohol Abuse. 2020;46(6):671-683. doi:10.1080/00952990.2020.1778713
- Liebling D, Mehta N, Gulati A. Opioid screening practices in the cancer pain patient. J Palliat Med. 2019;22(1):10-17. doi:10.1089/jpm.2018.0168
- Dans M, Kutner JS, Agarwal R, et al. NCCN Guidelines(R) Insights: Palliative Care, Version 2.2021. J Natl Compr Canc Netw. 2021;19(7):780-788. doi:10.6004/jnccn.2021.0033
- Kwon JH, Tanco K, Hui D, Reddy A, Bruera E. Chemical coping versus pseudoaddiction in patients with cancer pain. Palliat Support Care. 2014;12(5):413-417. doi:10.1017/S1478951513001351
- Anghelescu DL, Ehrentraut JH, Faughnan LG. Opioid misuse and abuse: risk assessment and management in patients with cancer pain. J Natl Compr Canc Netw. 2013;11(8):1023-1031. doi:10.6004/jnccn.2013.0120
- Marazziti D, Castrogiovanni P, Rossi A, et al. Pain threshold is reduced in depression. Int J Neuropsychopharmacol. 1998;1(1):45-48. doi:10.1017/S1461145798001047
- Tang J, Gibson SJ. A psychophysical evaluation of the relationship between trait anxiety, pain perception, and induced state anxiety. J Pain. 2005;6(9):612-619. doi:10.1016/j.jpain.2005.03.009
- Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964-973. doi:10.1016/j.jpain.2011.03.003
- Schneider E, Linden M, Weigmann H, et al. Early reduction in painful physical symptoms is associated with improvements in long-term depression outcomes in patients treated with duloxetine. BMC Psychiatry. 2011;11:150.
- ASCO Guidelines: Screening, Assessment, and Care of Anxiety and Depressive Symptoms in Adults with Cancer. American Society of Clinical Oncology. Published 2014. Accessed Month, day 2022. https://bit.ly/3RUg060
- Butler SF, Budman SH, Fernandez KC, Fanciullo GJ, Jamison RN. Cross-validation of a screener to predict opioid misuse in chronic pain patients (SOAPP-R). J Addict Med. 2009;3(2):66-73. doi:10.1097/ADM.0b013e31818e41da
- Reyes-Gibby CC, Anderson KO, Todd KH. Risk for opioid misuse among emergency department cancer patients. Acad Emerg Med. 2016;23(2):151-158. doi:10.1111/acem.12861
- Yennurajalingam S, Edwards T, Arthur JA, et al. Predicting the risk for aberrant opioid use behavior in patients receiving outpatient supportive care consultation at a comprehensive cancer center. Cancer. 2018;124(19):3942-3949. doi:10.1002/cncr.31670
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208-1217. doi:10.1111/j.1530-0277.2007.00403.x
- Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170(13):1155-1160. doi:10.1001/archinternmed.2010.140
- Prescription Opioids DrugFacts. National Institutes of Health. Published June 2021. Accessed June 15, 2022. https://bit.ly/3Bbac1K
- Kwon JH, Hui D, Bruera E. A pilot study to define chemical coping in cancer patients using the delphi method. J Palliat Med. 2015;18(8):703-706. doi:10.1089/jpm.2014.0446
- Strasser F, Walker P, Bruera E. Palliative pain management: when both pain and suffering hurt. J Palliat Care. 2005;21(2):69-79.
- Nguyen LM, Rhondali W, De la Cruz M, et al. Frequency and predictors of patient deviation from prescribed opioids and barriers to opioid pain management in patients with advanced cancer. J Pain Symptom Manage. 2013;45(3):506-516. doi:10.1016/j.jpainsymman.2012.02.023
- Del Fabbro E. Assessment and management of chemical coping in patients with cancer. J Clin Oncol. 2014;32(16):1734-1738. doi:10.1200/JCO.2013.52.5170
- Pergolizzi JV Jr, Magnusson P, Christo PJ, et al. Opioid therapy in cancer patients and survivors at risk of addiction, misuse or complex dependency. Front Pain Res (Lausanne). 2021;2:691720. doi:10.3389/fpain.2021.691720
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Weissman DE, Haddox DJ. Opioid pseudoaddiction: an iatrogenic syndrome. Pain. 1989;36(3):363-366. doi:10.1016/0304-3959(89)90097-3
- Dydyk AM, Jain NK, Gupta M. Opioid use disorder. In: StatPearls [Internet]. StatPearls Publishing; 2022. Accessed March 7, 2022. https://bit.ly/3Owa6ou
- Johnson RE, Strain EC, Amass L. Buprenorphine: how to use it right. Drug Alcohol Depend. 2003;70(suppl 2):S59-S77. doi:10.1016/s0376-8716(03)00060-7
- Dezman ZDW, Felemban W, Bontempo LJ, Wish ED. Evidence of fentanyl use is common and frequently missed in a cross-sectional study of emergency department patients in Baltimore, Maryland. Clin Toxicol (Phila). 2020;58(1):59-61. doi:10.1080/15563650.2019.1605078
- Castaneda AM, Lee CS, Kim YC, Lee D, Moon JY. Addressing opioid-related chemical coping in long-term opioid therapy for chronic noncancer pain: a multicenter, observational, cross-sectional study. J Clin Med. 2018;7(10):354. doi:10.3390/jcm7100354
- Yennurajalingam S, Arthur J, Reddy S, et al. Frequency of and factors associated with nonmedical opioid use behavior among patients with cancer receiving opioids for cancer pain. JAMA Oncol. 2021;7(3):404-411. doi:10.1001/jamaoncol.2020.6789
- Bruera E, Paice JA. Cancer pain management: safe and effective use of opioids. Am Soc Clin Oncol Educ Book. 2015:e593-e599. doi:10.14694/EdBook_AM.2015.35.e593
- Rahimi R, Nikfar S, Rezaie A, Abdollahi M. Efficacy of tricyclic antidepressants in irritable bowel syndrome: a meta-analysis. World J Gastroenterol. 2009;15(13):1548-1553. doi:10.3748/wjg.15.1548
- Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev. 2014(1):CD007115. doi:10.1002/14651858.CD007115.pub3
- Smith EM, Pang H, Cirrincione C, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA. 2013;309(13):1359-1367. doi:10.1001/jama.2013.2813
- Wiese B, Wilson-Poe AR. Emerging evidence for cannabis' role in opioid use disorder. Cannabis Cannabinoid Res. 2018;3(1):179-189. doi:10.1089/can.2018.0022
- Suzuki J, Weiss RD. Cannabinoids for the treatment of opioid use disorder: where is the evidence? J Addict Med. 2021;15(2):91-92. doi:10.1097/ADM.0000000000000711
- Kircher S, Zacny J, Apfelbaum SM, et al. Understanding and treating opioid addiction in a patient with cancer pain. J Pain. 2011;12(10):1025-1031. doi:10.1016/j.jpain.2011.07.006
- Taylor JL, Johnson S, Cruz R, Gray JR, Schiff D, Bagley SM. Integrating harm reduction into outpatient opioid use disorder treatment settings: harm reduction in outpatient addiction treatment. J Gen Intern Med. 2021;36(12):3810-3819. doi:10.1007/s11606-021-06904-4
- Kantor TG, Cantor R, Tom E. A study of hospitalized surgical patients on methadone maintenance. Drug Alcohol Depend. 1980;6(3):163-173. doi:10.1016/0376-8716(80)90455-x
- Manfredi PL, Gonzales GR, Cheville AL, Kornick C, Payne R. Methadone analgesia in cancer pain patients on chronic methadone maintenance therapy. J Pain Symptom Manage. 2001;21(2):169-174. doi:10.1016/s0885-3924(00)00252-9
- Karasz A, Zallman L, Berg K, Gourevitch M, Selwyn P, Arnsten JH. The experience of chronic severe pain in patients undergoing methadone maintenance treatment. J Pain Symptom Manage. 2004;28(5):517-525. doi:10.1016/j.jpainsymman.2004.02.025
- Edens EL, Abelleira A, Declan B, Becker WC. You say pain. I say addiction. Let’s call the whole thing off. Psychiatric Times. Published November 9, 2020. Accessed March 7, 2022. https://bit.ly/3v8bN4T
- Hanna V, Senderovich H. Methadone in pain management: a systematic review. J Pain. 2021;22(3):233-245. doi:10.1016/j.jpain.2020.04.004
- Mooney LJ. Medication treatment for opioid use disorder reduces suicide risk. Am J Psychiatry. 2022;179(4):262-263. doi:10.1176/appi.ajp.20220173
- Wakeman SE, Larochelle MR, Ameli O, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020;3(2):e1920622. doi:10.1001/jamanetworkopen.2019.20622
- Ahn MH, Park S, Lee HB, et al. Suicide in cancer patients within the first year of diagnosis. Psychooncology. 2015;24(5):601-607. doi:10.1002/pon.3705
- Merlin JS, Khodyakov D, Arnold R, et al. Expert panel consensus on management of advanced cancer-related pain in individuals with opioid use disorder. JAMA Netw Open. 2021;4(12):e2139968. doi:10.1001/jamanetworkopen.2021.39968
- Neumann AM, Blondell RD, Jaanimagi U, et al. A preliminary study comparing methadone and buprenorphine in patients with chronic pain and coexistent opioid addiction. J Addict Dis. 2013;32(1):68-78. doi:10.1080/10550887.2012.759872
- Suen LW, Lee TG, Silva M, et al. Rapid overlap initiation protocol using low dose buprenorphine for opioid use disorder treatment in an outpatient setting: a case series. J Addict Med. Published online February 10, 2022. doi:10.1097/ADM.0000000000000961
- Becker WC, Frank JW, Edens EL. Switching from high-dose, long-term opioids to buprenorphine: a case series. Ann Intern Med. 2020;173(1):70-71. doi:10.7326/L19-0725
- Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144(2):127-134. doi:10.7326/0003-4819-144-2-200601170-00010
- Thakrar AP. Short-acting opioids for hospitalized patients with opioid use disorder. JAMA Intern Med. 2022;182(3):247-248. doi:10.1001/jamainternmed.2021.8111
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.