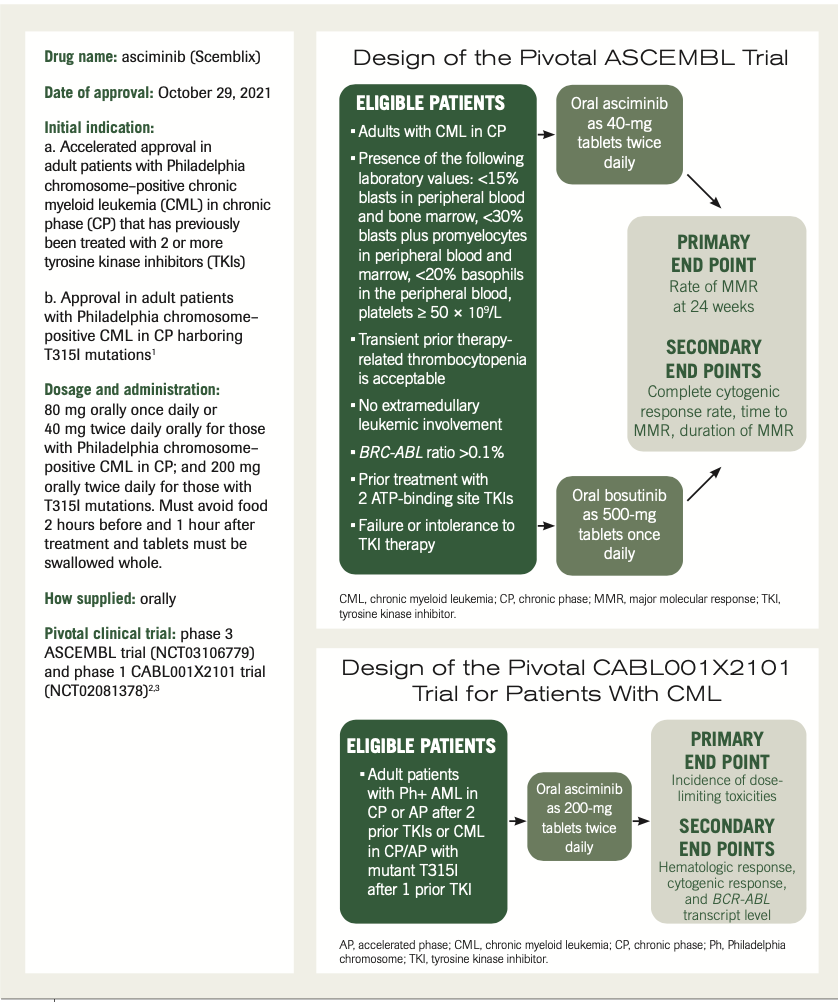
Expert Commentary on the Product Profile of Asciminib
In an interview with ONCOLOGY®, Elizabeth Travers, PharmD, BCOP, offers a comprehensive review of real-world treatment considerations of asciminib as therapy for patients with chronic myeloid leukemia.
Elizabeth Travers, PharmD, BCOP,
Clinical Pharmacist, Hematology/Blood and Marrow Transplant Pharmacist Assistant Professor
University of Kentucky College of Pharmacy
Lexington, Kentucky

Q: What is the mechanism of action of asciminib?
Travers: TKIs are effective drugs for the treatment of CML. In general, they work by inhibiting the transphosphorylation of BCR-ABL oncoproteins by binding to the ATP [adenosine triphosphate] binding site of the protein kinases, [which help to] prevent the protein fusion that causes CML. Resistance to TKIs is driven by point mutations in the ABL kinase domain.
Asciminib has a unique mechanism of action and is a first-in-class STAMP inhibitor. STAMP stands for Specifically Targeting the ABL Myristoyl Pocket. [Asciminib] is able to potently inhibit ABL kinase activity on that BCR-ABL fusion protein by allosterically binding to the ABL myristoyl pocket. It doesn’t compete with ATP and binds to a completely different pocket on that BCR-ABL, which gives it a few advantages over other TKIs. It’s less susceptible to mutations that drive resistance to TKIs. It also has less toxicity because it’s not targeting other kinases. In clinical trials, asciminib demonstrated activity against both wild-type BCR-ABL and several mutant forms, including T315I, and it even [showed] activity in heavily pretreated patients.
Q: What are the biggest concerns with the toxicity profile of asciminib? Have any new safety concerns become more apparent in the real-world setting?
Travers: Asciminib appears to be well tolerated, especially compared with other TKIs. Between the 2 major trials that led to the FDA approval, the most common adverse [effects; AEs] seen were upper respiratory tract infections, musculoskeletal pain, fatigue, nausea, rash, and diarrhea.4 Those occurred in more than 20% of patients. They also saw some common laboratory abnormalities such as decreased blood counts, including platelets, neutrophils, and hemoglobin. They also saw increases in triglycerides, creatinine kinase, liver enzymes, and pancreatic enzymes. Asciminib does contain warnings for myelosuppression, pancreatic toxicity, hypertension, hypersensitivity, and cardiovascular toxicity.
It’s important to note that the dosing of asciminib does vary based on indication. Patients who have mutated forms and T315I receive higher doses of asciminib than those with just CP-CML. The toxicity profile does vary a bit between those 2 dose levels.
In the ASCEMBL trial, which [included] patients with CP-CML who had received multiple TKIs—so, patients on an 80-mg total daily dose—they saw dose interruptions due to adverse drug reactions in 38% of patients and permanent discontinuation from drug events in 7%. Most of those interactions and discontinuation were due to hematologic toxicities. They did find in that study that the number of patients who discontinued treatment due to AEs was 3 times lower in the asciminib arm compared with the control arm [taking] bosutinib [Bosulif], at 7% vs 25%, showing better tolerability compared [with some of the currently available] TKIs.
In the phase 1 study [of patients with T315I-mutated CML], they saw dose interruptions in 31% of patients and permanent discontinuations due to drug events in 10% of patients. At the higher dose, [clinicians saw] slightly more discontinuations, and most of those were due to increases in pancreatic enzymes vs the hematologic toxicity that they see more commonly in the lower doses.
Q: Are dosing modifications common with this agent?
Travers: The package insert does include those recommendations for modifications for both first and subsequent dose reductions. Those specific recommendations vary, depending on the indication and starting dose. The package insert does contain dose reductions for myelosuppression and asymptomatic amylase and lipase elevations. In patients in clinical trials on the 80-mg daily dose, dose reductions of asciminib due to AEs [occurred] in 7% of patients. Most of those who required dose adjustments [had developed] thrombocytopenia and neutropenia. Patients on the 400-mg daily dose needed dose reductions for AEs [at a rate of 23%]. Those were for a wider variety of reasons; pancreatic enzyme elevations were the most common at 10%, followed by abdominal pain, anemia, increased bilirubin, dizziness, fatigue, and increased [liver function enzymes]. We see a wider range of toxicity with a higher dose requiring dose modifications. In our experience, we have not needed [dose modifications], yet.
Q: What are the major drug interactions clinicians should be aware of, if any?
Travers: Asciminib itself is a CYP3A4 [cytochrome P450 3A4] substrate. When you’re using it with a strong CYP3A4 inhibitor, it will increase your asciminib Cmax and AUC [area under the curve], increasing the risk of AEs. The package insert does recommend that patients on the higher 400-mg total daily dose and a strong CYP3A4 inhibitor to be closely monitored for AEs.
Asciminib is also a CYP3A4 inhibitor, so it can increase AEs when given with CYP3A4 substrates. Patients on the 80-mg total daily dose need to be closely monitored, but [the manufacturer does] recommend avoiding the 400-mg daily dose with certain CYP3A4 substrates. In addition to impacting CYP3A4, asciminib is also a CYP2C9 inhibitor. It’s recommended to avoid coadministration of asciminib with some CYP2C9 substrates, and if administration is unavoidable, you need to reduce that CYP2C9 substrate dosage as recommended in that drugs package insert. I also want to mention that the AUC and Cmax of asciminib are decreased by 62% and 68%, [respectively], when taken with a high-fat meal, so it’s important to counsel patients to take this medication on an empty stomach. You need to avoid food for 2 hours before and 1 hour after asciminib administration.
Q: Have any barriers to administration or receipt by the patient emerged since this agent’s approval?
Travers: With asciminib being so new and being a specialty medication, it does need to be filled through a specialty pharmacy. Luckily, it doesn’t appear to be restricted in distribution to any specific pharmacy unless your patient’s insurance dictates they have to fill it somewhere specifically. Our specialty pharmacy has been able to obtain asciminib for several patients. They haven’t run into any issues with insurance authorization, and most plans seem to be covering it as long as we’re prescribing within that FDA-approved labeling. We’ve been able to easily fill the drug for patients on Medicare, Medicaid, and those with private insurance. For the small number of patients we personally had on it, the co-pay seems to be reasonable, but that can greatly vary by insurance plan. For patients needing additional financial assistance, Novartis, asciminib’s manufacturer, has several patient assistance programs available. They have the Novartis [Oncology] Universal Co-pay Program, and they have a 30-day voucher that can help eligible patients start therapy quickly. They [also] have a Patient Assistance support center, which has insurance specialists and case managers who can help your patients find financial resources that are available for their medications.
Q: Would you like to add anything else?
Travers: Asciminib provides us with a great novel mechanism for treating CML, and it particularly has a niche for patients who are unable to tolerate the other TKIs due to AEs or patients whose CML progressed due to mutations. However, asciminib is only FDA approved for CP-CML. I’ve found that many of our patients who have failed the other 5 commercially available TKIs wind up progressing into accelerated phase [AP] or blast phase [BP] at some point during their treatment. Unfortunately, given that asciminib has not been significantly studied outside of CP-CML, we don’t have any data for safety or efficacy in AP or BP. Of the 150 patients with CML in the phase 1 study, only 9 had AP disease and none were included in the phase 3 ASCEMBL trial that led to the FDA approval. Until studies are done in the AP and BP population, it can be hard to recommend asciminib for these patients. It will be even more difficult to get someone’s insurance to pay for an off-label use of such a brand-new medication.
Design of the Pivotal ASCEMBL Trial and the CABL001X2101 Trial for Patients With CML
REFERENCES
- Scemblix. Prescribing information. Novartis; 2021. Accessed March 18, 2022. https://bit.ly/3wl250i
- Réa D, Mauro MJ, Boquimpani C, et al. A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021;138(21):2031-2041. doi:10.1182/blood.2020009984
- Cortes JE, Hughes TP, Mauro MJ, et al. Asciminib, a first-in-class STAMP inhibitor, provides durable molecular response in patients (pts) with chronic myeloid leukemia (CML) harboring the T315I mutation: primary efficacy and safety results from a phase 1 trial. Blood. 2020;136(suppl 1):47-50. doi:10.1182/blood-2020-139677
- FDA approves asciminib for Philadelphia chromosome–positive chronic myeloid leukemia. October 29, 2021. Accessed March 18, 2022. https://bit.ly/3wzKpyj