The Prognostic Significance of Peripheral Blood Biomarkers in Patients With Advanced Non–Small Cell Lung Cancer Treated With Pembrolizumab: A Clinical Study
Kira MacDougall, MD, and co-investigators, research the importance of peripheral biomarkers in patients with advanced non–small cell lung cancer who are treated with pembrolizumab.
ABSTRACT
Systemic inflammation has long been associated with poor outcomes in many types of solid tumors. Peripheral blood biomarkers, such as absolute lymphocyte count (ALC) and the ratio of absolute neutrophil count to absolute lymphocyte count (ANC/ALC), have been shown to be immune-inflammatory parameters highlighting an individual’s immune status. The prognostic role of ALC and ANC/ALC on overall survival (OS) was examined in patients with advanced non–small cell lung carcinoma (NSCLC) receiving pembrolizumab. Of a total of 239 patients, 52% were male, with a median age of 67 years (interquartile range [IQR], 59-73). Most patients had a diagnosis of adenocarcinoma (76%), with stage IV disease (82%). PD-L1 expression was >50% in 44% of the patients. The median time on treatment with pembrolizumab was 5.8 months (IQR, 2.9-12.7). An ANC/ALC <5 was associated with improved OS at initiation of pembrolizumab (P = .002), whereas an ALC >1.4 deciliter (dL) trended toward improved OS compared with ALC <1.4 dL (P = .053). After adjusting for potential cofounders with a multivariate analysis, a baseline ANC/ALC of 5 or higher was associated with a significantly increased risk of death (HR, 1.93; 95% CI, 1.27-2.93; P = .002). An ANC/ALC <5 at the time of initiation of treatment with pembrolizumab was associated with improved OS in patients with advanced NSCLC. The median ALC and ANC/ALC were significantly lower after 6 weeks of treatment with pembrolizumab.
Keywords: pembrolizumab; non–small cell lung cancer; absolute lymphocyte count; absolute neutrophil count to absolute lymphocyte count ratio; immunotherapy; peripheral blood counts; anti–PD-1
Oncology (Williston Park). 2022;36(3):156-161.
DOI: 10.46883/25920954
Introduction
Lung cancer is the most common cause of cancer-related deaths, both in the United States and internationally.1,2 Non–small cell lung cancer (NSCLC) accounts for approximately 80% to 85% of these cases. The discovery of immune checkpoint inhibitor therapy has led to significant improvement in both overall survival (OS) and progression-free survival (PFS) and represents a paradigm shift in treatment of NSCLC. In 2019, 2 anti–PD-1 antibodies, pembrolizumab (Keytruda) and nivolumab (Opdivo), and 1 anti–PD-L1 antibody, atezolizumab, were approved by the FDA for the treatment of metastatic NSCLC.3 PD-1 is an immune checkpoint transmembrane protein that is expressed on macrophages, dendritic cells, and T and B lymphocytes. When PD-1 binds to one of its ligands that are expressed on human cancer cells— PD-L1 or PD-L2—it inhibits cytotoxic T-cell response and evades the body’s immune surveillance system.4,5
While PD-L1 receptor positivity in tumor cells has been shown to predict the responsiveness of the cancer to these agents, it has its limitations. Several small studies have been performed to assess the utility of hematologic biomarkers in predicting the effectiveness of immunotherapy. However, these studies have been small retrospective studies with small sample sizes. These peripheral markers include absolute neutrophil count (ANC), absolute lymphocyte count (ALC), the ratio of absolute neutrophil count to absolute lymphocyte count (ANC/ALC), absolute eosinophil count, and absolute monocyte count (AMC). These biomarkers have been shown to be immune-inflammatory parameters highlighting an individual’s immune status. Aggressive cancers are associated with an increased systemic inflammatory state, creating a microenvironment that promotes angiogenesis, survival of malignant cells, and metastasis. The response to immunotherapy in these cases is poor.6 Therefore, this question has arisen: Can these peripheral blood biomarkers predict patient outcomes in patients treated with immunotherapy?
The aim of this study is to investigate ALC and ANC/ALC in patients with advanced NSCLC receiving pembrolizumab and to determine if a correlation exists between these key biomarkers and OS. To our knowledge, of studies investigating this relationship, this is the largest in terms of number of patients with NSCLC treated with pembrolizumab.
Methods
Patient Selection
This retrospective observational study was approved by the Northwell Health Institutional Review Board, which waived the requirement for informed consent. Data for all patients with advanced NSCLC treated with pembrolizumab between September 2016 and May 2020 at Northwell Health hospital sites were collected by reviewing their electronic medical records. Patients treated with immunotherapy other than pembrolizumab were excluded. This helped to minimize heterogeneity related to different immunotherapy treatments.
Data Collection
All records were reviewed retrospectively and organized in the REDCap database. Parameters such as age at diagnosis, sex, histologic type, tumor PD-L1 status, stage of disease, line of treatment, history of radiation to the tumor, presence or absence of central nervous system (CNS) disease, and ECOG performance status were defined and adjusted for confounding. Peripheral blood counts including ALC, ANC, and AMC were examined at initiation of pembrolizumab and at 6 weeks on treatment. Patients without follow-up blood counts at 6 weeks were excluded.
Statistical Analysis
Based on literature review and previous studies that investigated this relationship, ANC/ALC cut-off values were ≥5 and <5, and ALC cut-off values were ≥1.4 dL and <1.4 dL. The primary outcome was OS, as defined as date of first dose of pembrolizumab to death or last follow-up. Patients discontinued their immunotherapy due to disease progression or death, or because they experienced adverse events (AEs). Descriptive statistics were used to present patient characteristics. Chi-square or Fisher’s exact test were used to compare categorical variables, and the Wilcoxon-Mann-Whitney test was used to compare continuous variables. OS rates were plotted on Kaplan-Meier curves and differences were evaluated with the log-rank test. A multivariable Cox regression model was used to determine the effect of baseline ANC/ALC on the risk of death after adjusting for potential confounders. All statistical tests were 2-sided and conducted using SPSS version 25.0 (IBM). P <.05 was considered statistically significant.
Results
Patient Characteristics
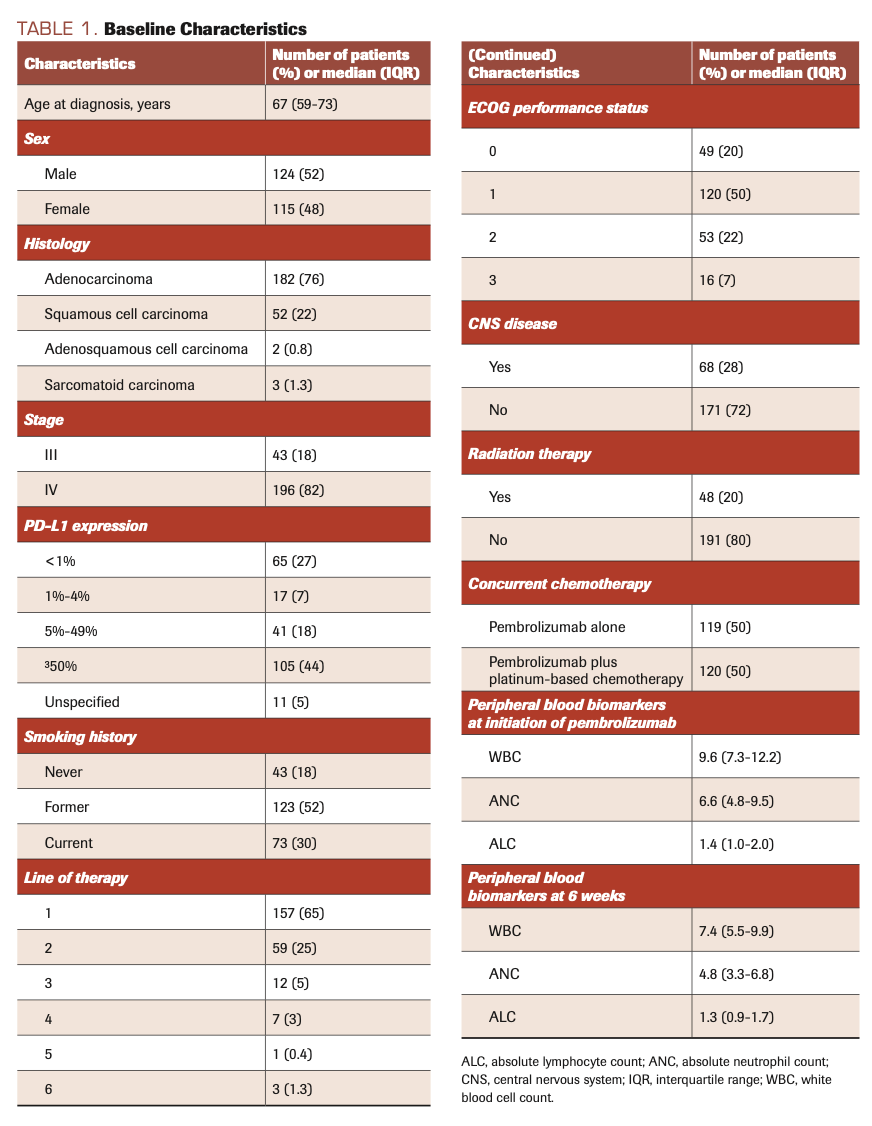
A total of 239 patients with advanced NSCLC treated with pembrolizumab at Northwell Health hospital centers were included. Baseline characteristics are presented in Table 1. Median age at diagnosis was 67 years (interquartile range [IQR], 59-73). Of all patients, 52% were male and most (76%) had a diagnosis of adenocarcinoma, with stage IV disease (82%). The majority (52%) of the included patients were former smokers. PD-L1 expression was >50% in 44% of the patients. ECOG performance status was 0 or 1 in 70% of patients. Radiographic evidence of CNS disease at the time of pembrolizumab therapy was present in 28% of patients, and 20% had received radiation therapy to the tumor prior to the initiation of pembrolizumab. Pembrolizumab was first-line therapy in 65% of patients. Pembrolizumab monotherapy was being used for treatment in 119 patients (50%), whereas 120 patients (50%) received a combination of pembrolizumab plus platinum-based chemotherapy.
TABLE 1. Baseline Characteristics
Comparison of Peripheral Blood Biomarkers at Baseline and at 6 Weeks of Treatment
The median ALC and ANC/ALC ratio were significantly lower after 6 weeks of pembrolizumab therapy compared with the start date of treatment (1.3 dL [IQR, 0.9-1.7] vs 1.4 dL [IQR, 1.0-2.0]; P <.001, and 3.6 [IQR, 2.1-6.1] vs 4.6 [IQR, 2.8-7.0] respectively; P = .002).
Comparison of OS Based on Baseline Peripheral Blood Biomarkers
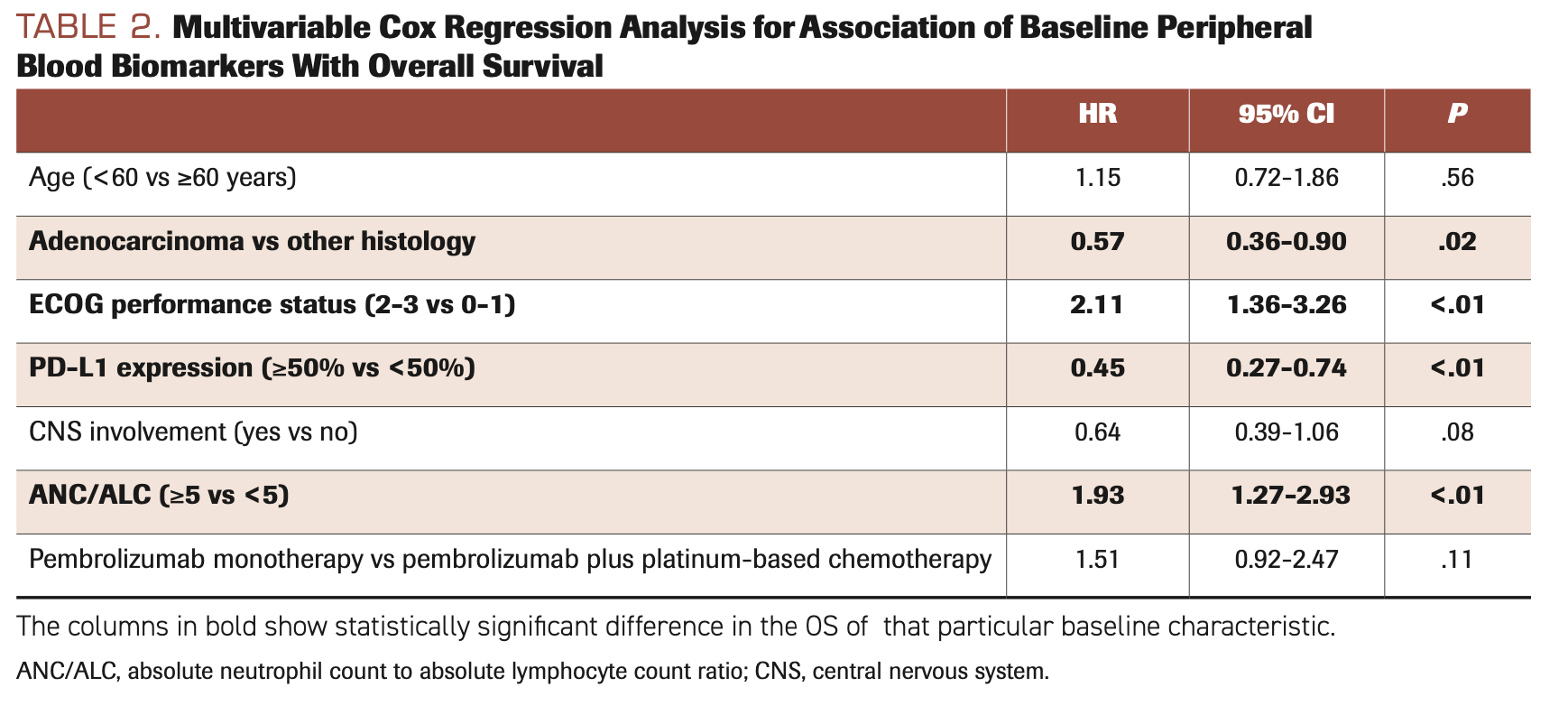
Median OS was 10.8 months (IQR, 4.9-17.4) and overall time on treatment was 5.8 months (IQR, 2.9-12.7). An ALC of ≥1.4 dL trended toward improved OS compared with ALC <1.4 dL (P = .053) (Figure A). Patients with a baseline ANC/ALC of ≥5 had a worse median OS rate compared with those with ANC/ALC <5, at 8.8 months (IQR, 3.98-15.65) vs 11.75 months (IQR, 6.68-20.51; P = .02) (Figure B), and after adjusting for potential cofounders in multivariate analysis (HR, 1.93; 95% CI, 1.27-2.93; P = .002) (Table 2). There was no difference in OS in patients who received pembrolizumab monotherapy compared with those who received pembrolizumab plus platinum-based chemotherapy (HR, 1.51; 95% CI, 0.92-2.47; P = .11).
FIGURE. Kaplan-Meier Survival Estimates Between Groups With Different ANC/ALC Ratio and ALC Ratio at the Start Date of Pembrolizumab
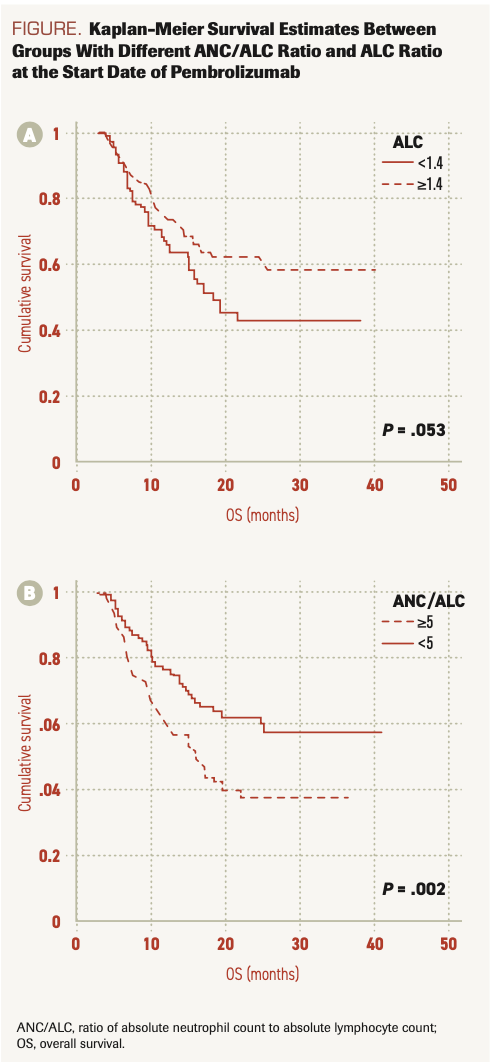
TABLE 2. Multivariable Cox Regression Analysis for Association of Baseline Peripheral Blood Biomarkers With Overall Survival
Discussion
This is the largest study analyzing the effect of the baseline serum levels of ANC and ALC, and of the ANC/ALC ratio, on the OS of patients treated with pembrolizumab for NSCLC. We show here that patients with an ALC of ≥1.4 dL and an ANC/ALC ratio <5 at the initiation of pembrolizumab therapy had an improved OS compared with their respective counterparts. After adjusting for potential cofounders, we found that patients with baseline ANC/ALC ratio of ≥5 treated with pembrolizumab had almost 2 times increased risk of death (all-cause mortality) (HR, 1.93; 95% CI, 1.27-2.93), compared with those with a baseline ANC/ALC <5.
Our findings are consistent with those of previous studies on peripheral blood biomarkers in patients being treated with anti–PD-1 antibodies. In a metanalysis of 16 studies that included 1700 patients, a high blood neutrophil-to-lymphocyte ratio (NLR) or ANC/ALC was found to be associated with shorter OS and PFS in patients getting treatment with PD-1/PD-L1 inhibitors for NSCLC.7 In a retrospective study of 22 patients with NSCLC treated with nivolumab, baseline ALC levels and ANC/ALC ratios were positively and negatively correlated, respectively, with OS on nivolumab.8 Another study of 109 patients with advanced NSCLC treated with nivolumab found that posttreatment ANC/ALC ≥5 after 2 cycles of nivolumab was associated with poor OS.9 Soyano et al studied this effect in patients treated with nivolumab (n = 146) and pembrolizumab (n = 11), finding that a baseline ANC/ALC ratio of 5.9 or more was associated with a significantly increased risk of death (HR, 1.94; 95% CI, 1.24-3.03; P = .004).10 Hasegawa et al demonstrated that high NLR (>4.55) at the pretreatment stage was significantly associated with shorter PFS and OS in a study of 51 patients with NSCLC who had a tumor proportion score >49%.11 Unlike our study, this was studied solely in patients who received pembrolizumab monotherapy. Zer et al studied these peripheral biomarkers in correlation with OS, disease control rate, and time to progression, and they found improved outcomes in patients with NLR of ≤4, in the patients with NSCLC who were under treatment with PD-1/PD-L1 for NSCLC.12
The results of several studies have shown that tumor-related neutrophils are predictive of a poor prognosis in patients with malignancies. These neutrophils are attracted by cytokines such as interleukin-8 (IL-8), which further promotes the angiogenesis, local invasion of vessels, and growth factor release that causes metastatic spread of disease, leading to poor outcomes.13,14 One study demonstrated that lung carcinomas release IL-6 and granulocyte monocyte colony-stimulating factor that leads to increased peripheral leukocyte count, predicting ominous outcomes.15 PD-1/PD-L1 inhibitors act by blocking the interaction of negative regulators of T-cells that increase the antitumor immunity and decreases the antitumor immune tolerance, and it is plausible that these changes alter the count of peripheral neutrophils and lymphocytes. Increased peripheral neutrophil count correlates with reduced CD8-positive T-lymphocyte counts in NSCLC, and lymphopenia reflects impaired cellular immune response.16,17 Conversely, high lymphocyte counts have been considered a positive prognostic factor due to an improved antigen-driven immune response. The exact mechanism by which NLR affects immunotherapy or checkpoint blockade is not known, but it has been repeatedly shown to be associated with better outcomes in malignancies and other systemic diseases.
The use of PD-1 and PD-L1 inhibitors have revolutionized cancer immunotherapy and have led to improvement in patient outcomes. Their effect, however, seems to be limited to certain patient subgroups. Given the significant immune-related AEs that can occur with these drugs, along with their financial toxicity, there is a need to individualize treatment for every single patient. Tumor PD-L1 immunohistochemical testing is often used as a predictor of response, but it has limitations. Complete blood count measures and differential testing are inexpensive and routinely performed before the initiation of immunotherapy and before every treatment cycle.
Limitations
This study sought to determine the usefulness of hematologic biomarkers in predicting patient outcomes. However, it did have limitations due to its retrospective study design. Concurrent inflammatory states and use of immunomodulatory agents or steroids could not be ruled out; these could alter the cell counts. Furthermore, the ANC/ALC could not be assessed separately at the tumor site and could differ from that of the peripheral blood. Future studies should be designed to address these issues.
Conclusions
An ANC/ALC <5 at the time of initiation of treatment with pembrolizumab was associated with improved OS in patients with advanced NSCLC. However, further prospective studies are warranted to establish if ANC/ALC can be reliably used as a predictive biomarker in patients with advanced NSCLC who are treated with immunotherapy.
Author Affiliations:
Kira MacDougall, MD1; Muhammad Rafay Khan Niazi, MD2; Jeff Hosry, MD2; Sylvester Homsy, MD3; Alexander Bershadskiy, MD4
1Department of Hematology & Medical Oncology, Oklahoma University of Health Sciences, Oklahoma City, OK, USA
2Department of Internal Medicine, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, Staten Island, NY, USA
3Department of Hematology & Medical Oncology, SUNY Downstate Medical Center, Brooklyn, NY, USA
4Division of Hematology & Medical Oncology, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, New York, NY, USA
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5-29. doi:10.3322/caac.21254
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69-90. doi:10.3322/caac.20107
- Langer CJ, Gadgeel SM, Borghaei H, et al; KEYNOTE-021 Investigators. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016;17(11):1497-1508. doi:10.1016/S1470-2045(16)30498-3
- Rafei H, El-Bahesh E, Finianos A, Nassereddine S, Tabbara I. Immune-based therapies for non-small cell lung cancer. Anticancer Res. 2017;37(2):377-387. doi:10.21873/anticanres.11330
- Wherry EJ. T cell exhaustion. Nat Immunol. 2011;12(6):492-499. doi:10.1038/ni.2035
- Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436-444. doi:10.1038/nature07205
- Jiang T, Bai Y, Zhou F, et al. Clinical value of neutrophil-to-lymphocyte ratio in patients with non-small-cell lung cancer treated with PD-1/PD-L1 inhibitors. Lung Cancer. 2019;130:76-83. doi:10.1016/j.lungcan.2019.02.009
- Karantanos T, Karanika S, Seth B, Gignac G. The absolute lymphocyte count can predict the overall survival of patients with non-small cell lung cancer on nivolumab: a clinical study. Clin Transl Oncol. 2019;21(2):206-212. doi:10.1007/s12094-018-1908-2
- Khunger M, Patil PD, Khunger A, et al. Post-treatment changes in hematological parameters predict response to nivolumab monotherapy in non-small cell lung cancer patients. PLoS One. 2018;13(10):e0197743. doi:10.1371/journal.pone.0197743
- Soyano AE, Dholaria B, Marin-Acevedo JA, et al. Peripheral blood biomarkers correlate with outcomes in advanced non-small cell lung cancer patients treated with anti-PD-1 antibodies. J Immunother Cancer. 2018;6(1):129. doi:10.1186/s40425-018-0447-2
- Hasegawa T, Yanagitani N, Utsumi H, et al. Association of high neutrophil-to-lymphocyte ratio with poor outcomes of pembrolizumab therapy in high-PD-L1-expressing non-small cell lung cancer. Anticancer Res. 2019;39(12):6851-6857. doi:10.21873/anticanres.13902
- Zer A, Sung MR, Walia P, et al. Correlation of neutrophil to lymphocyte ratio and absolute neutrophil count with outcomes with PD-1 axis inhibitors in patients with advanced non-small-cell lung cancer. Clin Lung Cancer. 2018;19(5):426-434.e1. doi:10.1016/j.cllc.2018.04.008
- Hagerling C, Werb Z. Neutrophils: critical components in experimental animal models of cancer. Semin Immunol. 2016;28(2):197-204. doi:10.1016/j.smim.2016.02.003
- Moses K, Brandau S. Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol. 2016;28(2):187-196. doi:10.1016/j.smim.2016.03.018
- Kasuga I, Makino S, Kiyokawa H, Katoh H, Ebihara Y, Ohyashiki K. Tumor-related leukocytosis is linked with poor prognosis in patients with lung carcinoma. Cancer. 2001;92(9):2399-2405. doi:10.1002/1097-0142(20011101)92:9<2399::aid-cncr1588>3.0.co;2-w
- Kargl J, Busch SE, Yang GHY et al. Neutrophils dominate the immune cell composition in non-small cell lung cancer. Nat Commun. 2017;8:14381. doi:10.1038/ncomms14381
- Gooden MJM, de Bock GH, Leffers N, Daemen T, Nijman HW. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer. 2011;105(1):93-103. doi:10.1038/bjc.2011.189