Learning AE Management With Immunotherapy vs TKIs in RCC
Hans Hammers, MD, and his team discuss the most pertinent treatment options for patients with renal cell carcinoma.
Hans Hammers, MD, and his team discuss the most pertinent treatment options for patients with renal cell carcinoma.
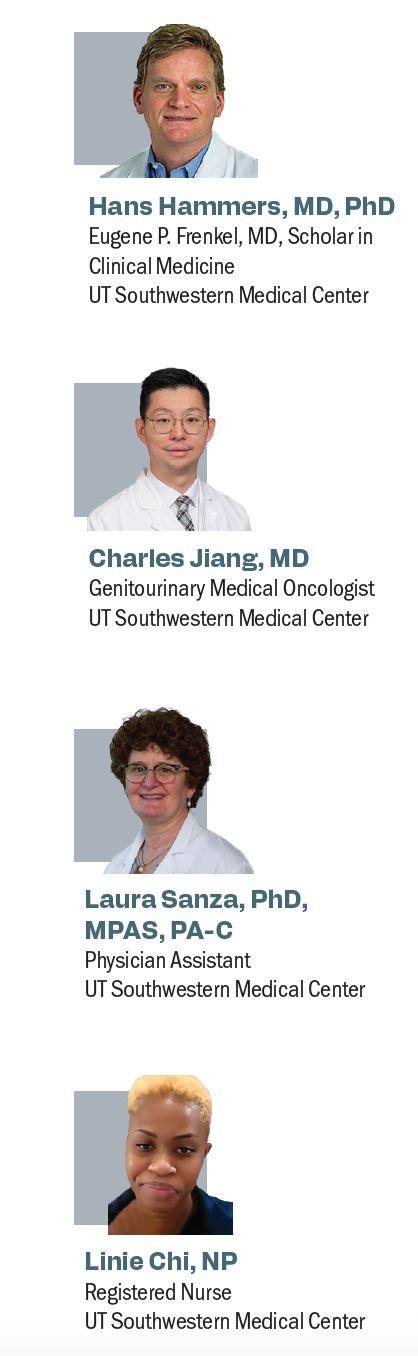
During an Around the Practice Program®, Hans Hammers, MD, PhD, and his colleagues sat down to discuss treatment options for those with advanced renal cell carcinoma (RCC). The discussion centered around immunotherapy vs tyrosine kinase inhibitors (TKIs), and adverse effect (AE) management.
Hammers was joined by Charles Jiang, MD; Laura Sanza, PhD, MPAS, PA-C; and Linie Chi, NP, all of whom work at UT Southwestern Medical Center and are part of the same treating team. Each expert contributed to a different part of the discussion focusing on treatment options in the space, patient management, and how to best control AEs and educate patients and caregivers.
Hammers / To begin, can you provide an overview of advanced RCC, such as the epidemiology and how it typically presents?
Jiang / As medical oncologists, we mostly see patients with advanced disease. I will say many cases are presented without any symptoms until they have an incidental finding and reveal they have a metastatic disease. [Patients] are most likely having some flank pain, hematuria, or a palpable abdominal mass. Other symptoms may present with weight loss, fever, night sweats, fatigue, or anemia. Quite unspecific; I will say the most common patients were older, probably 50 or 60 years old, and they’re mostly male patients. We do see some patients with the occasional family history, accounting for about 5% to 10% of the cases. The other thing we see a lot is the patient smoked, or they were obese, and had hypertension, or kidney disease, or some sort of genetic symptoms such as von Hippel-Lindau disease.
Hammers / These days, we find RCC most of the time serendipitously by getting imaging studies for completely different reasons. Most of the time, we don’t find patients anymore presenting with metastatic disease; most of the time, patients present with stage III disease, for example, or earlier stage disease, and they get a nephrectomy. That is another way we see patients; we may see patients without any evidence of disease burden. For patients who had a considerable risk of recurrence typically in stage III, the risk of recurrence is 30% to 50%. Over the next 5 years, we will have adjuvant therapy now in that space. Dr Jiang, what do you think about adjuvant therapy? What is available for this landscape? Several trials have been placed in this space. What can you tell us about adjuvant therapy?
Jiang / For adjuvant therapy for RCC, we only had 1 option available for a long time, which was Sutent [sunitinib]. Nowadays, we’re excited to have a few more options. Pembrolizumab [Keytruda]—according to the phase 3 KEYNOTE-564 data [NCT03142334], presented at the 2024 American Society of Clinical Oncology Genitourinary [Cancers] Symposium, they updated their long-term result, suggesting these data—brought patients an overall survival benefit.1 I know a lot of people have different comments about this, about who has benefited, but at least according to this trial, they can show some benefit in the experimental group compared with the control arm. Similarly, we have another trial, phase 3 CheckMate 914 [NCT03138512].2 In that specific trial, they compared nivolumab [Opdivo] plus ipilimumab [Yervoy] vs nivolumab vs placebo study. That trial was unfortunately a negative study, and this spurred a lot of debate among [genitourinary] oncologists.
Hammers / The advantage of doing immunotherapy now is that you may avoid recurrence in a subset of patients where you could decrease the risk. All these tests are available, but I don’t think there is yet clear-cut evidence that we should use those or can use those and if they will hold value or be useful. That’s why we like immunotherapy in principle, because this is a potentially curative treatment option, even in patients with metastatic recurrence. It’s not like chemotherapy that only cures [patients] in the adjuvant space but not when the disease recurs. Immunotherapy may be active in any disease space. That’s the interesting component. How do we educate patients about their disease?
Sanza / We find educating the patient empowers them, and those who have ownership of what’s going on and are proactive do better [outcomes-wise]. The physician assistant [PA], whether it’s myself or one of my colleagues, sees a patient as they embark on treatment. Multiple things happen during that visit. It’s a little bit of a whirlwind. No. 1, I find repetition [is key]. Sometimes they’re so overwhelmed. I reiterate a lot of what the attending has said to the patient, and I like to explain to them again, like the mechanism of action [of the treatment], what the immunotherapy is doing. Having heard it from Dr Hammers on the medical level, and they hear a lot of medical terms, and then I explain it [at a] more grade 1 level, it starts to fall into place, and they start to understand, and they start to have a little bit of ownership.
I’ll review the profile of symptoms, and [AEs] to look for, which I know Dr Hammers goes into detail [about], and that might have been a lot of [information that wasn’t retained]; it starts to fall into place. Now the PA and the nurse, a combination team, 2 of us give handouts that talk about [TKIs], AEs, immunotherapy, adverse inflammation, inflammation of different parts of the body that we don’t want to be inflamed, what to look for, and when to report. The next thing I do is I read the situation. Are they by themselves? Do they have a lot of family support? What level should I be explaining things on? How much should I be writing out on lists? Do I draw pictures? These are all things that help tailor it to each patient.
The other thing I need to investigate in that very critical up-front visit is explaining logistics. I think the important message we try to give up front is that we’re going to follow them very closely and constantly review the toxicity. I think they’re reassured that while it’s important to understand what to look for, they don’t have to memorize it. They’re not going to get a test. The more we see them, they start to remember because we’ll ask the same questions. How is your blood pressure? How’s your appetite? How was your weight? Reassuring them that we’re going to see them often up front, read how well they’re doing. Then define when [they] should come back next. We have to put great effort into modulating the AEs. We will see them more often those who are tolerating [treatment] very well, then they can come back in a couple of weeks.
Hammers / Linie, you are at the forefront of patient communication. How do you make sure patients get the attention that they need?
Chi / If they just saw Dr Hammers and it’s a brand-new patient, I try to make sure that they have the 24/7 call center number. In some cases, depending on the patient, you have the older patients, sometimes I help punch it into the phone and have the numbers saved. Some of the patients [need help with the] MyChart app. I’ll help them set it up on [their] phone, or I’ll print out a sheet that gives them step-by-step directions. At the start of the visit, you can tell [which pateints] are hyper-independent people.… I try to find out who on the [patient’s] team is the leader, the pusher, who will suddenly push the patient to call or send the MyChart message. Half of the messages are sent by [spouses or children], or people who care.
If a patient sends a message and says, “FYI, just letting you know,” I’ll always call back those patients because I’m not sure why [they] sent it. Under the guidance of Dr Hammers, [Dr Jiang], whoever the provider is, patients get sent to the emergency department [ED] or our acute care clinic, which is a bridge between the ED and the provider. I’ve seen patients who would rather come into the acute care clinic than go into the ED. Half of the time, they know those providers, so they call the providers who are there by name. I always make sure if I’m seeing them there for the first time, I tell them that I talk with whoever the provider is. Immediately you see a [sigh] of relief, they’re like, “OK, you’re not just sending me to another doctor who has no idea what’s going on.” If we keep reiterating to them, “All you need to worry about is telling me what’s wrong, and then we’re going to handle telling you how to fix it.” They get nervous when they think about what’s wrong, and how to fix it. I tell them, “The first step is telling us what’s wrong, and all the other providers are going to tell you how to fix it.” That’s how I’m the gatekeeper to phone calls and MyChart messages.
Hammers / Is there a quality-of-life difference between TKIs and immunotherapy?
Sanza / There is a difference between the immunotherapy and the TKI toxicity. I do point out, to set expectations for the patient, that immunotherapy does not have to have any symptoms or problems to be meaningful and effective. They’re not hoping for it, because I’ve seen patients say, “Well, I hope I get immune-
mediated diarrhea so I know it’s working.”
Hammers / What are some common AEs associated with immunotherapy?
Sanza / They might have fatigue, maybe not eating as well. I would say those are mild. I have people [who are] just great, they’re working full time, they’re traveling, they can almost have no [AEs].
Hammers / I tell them all these horror stories on AEs like colitis, inflammation of the lung, brain, liver, everything from the top of the head to the toes. The truth is the most common AEs are exactly as you said, fatigue, skin rash, and itching, [which are] well tolerated. That is contrasted by what patients feel on TKIs on a daily basis.
Sanza / With TKIs, I set the expectation that they are going to notice fatigue, altered taste, and decreased appetite, which can translate to weight loss. They may have sensitivity, not just rash, but they may have sensitivity, blisters peeling on their hands and feet, which you will not see with immunotherapy, per se. They might have diarrhea with some of the TKIs, or with lenvatinib [Lenvima] you might have constipation. [They might have] an altered gastrointestinal tract, and in some patients that can translate to nausea. Setting the expectations that they’re going to be challenged with AEs scares [patients] sometimes, but then I reassure them that close monitoring and modulating the symptoms [are possible, and] we have them see an oncology dietitian to optimize their protein intake, to optimize their calorie intake.
We monitor their weight; we might have them see cardiologists in the cancer center who will help optimize their blood pressure. We will have them use Imodium [loperamide] on very specific regimens to control their diarrhea. Our goal is to hear and listen, what are the challenges to their functional status, what can we do with aggressive symptom management to mitigate that, and when we can’t always mitigate it enough that there is a functional decline, what can we introduce like brakes? Especially with the TKI, we introduced brakes so that it’s enough to soften the buildup of toxicity and symptoms but not enough to allow cancer to go out of control. We have found that sometimes that makes a difference, and things level off, and they get the reins back in their hands. They feel they’re in control again. After having a rough start with the TKI, [we can] do a good job of symptom management and introducing breaks, adequate to make a difference, but not enough to change the effectiveness. I’ve seen patients go on to travel on cruises and to other countries with TKIs in their pocket. Maybe we might have them orchestrate a break while they’re on vacation, only sometimes for about 3 to 5 days, and then they can restart, and they’ll be home by the time the symptoms start to build up.
Hammers / We tend to think that the TKIs give an additional layer of AEs that immunotherapy doesn’t have. The truth is these are manageable AEs. We can give the patient autonomy in managing [their disease]. I tend to dose reduce less than probably some other providers, and I rather use breaks. There are many different schedules to commit to. Some of our colleagues have mastered how to individualize these TKIs, dose titration, and adjustment. We can push these for longer, and that way we can optimize the outcome because the truth is, unfortunately, most patients will not respond to immunotherapy, or the immunotherapy component, and the masterful use of these agents is going to be important to prolong the benefit. Although they are palliative, they’re critical to keep our patients alive and potentially get them access to future therapies.
REFERENCES
- Choueiri TK, Tomczak P, Park SH, et al. Overall survival results from the phase 3 KEYNOTE-564 study of adjuvant pembrolizumab versus placebo for the treatment of clear cell renal cell carcinoma (ccRCC). J Clin Oncol. 2024;42(suppl 4):LBA359. doi.10.1200/JCO.2024.42.4_suppl.LBA359
- Motzer RJ, Bex A, Russo P, et al. Adjuvant nivolumab monotherapy vs placebo for localized renal cell carcinoma at high risk of relapse after nephrectomy: results from Part B of the randomized, phase 3 CheckMate 914 trial. J Clin Oncol. 2024;42(suppl 4):LBA358. doi.10.1200/JCO.2024.42.4_suppl.LBA358