Limited Resections May Have a Role in Localized Lung Cancer
NEW YORK-Interim results from an ongoing study of limited resections for some stage IA lung cancers are encouraging, a Japanese surgeon reported at the 3rd International Conference on Screening for Lung Cancer.
NEW YORKInterim results from an ongoing study of limited resections for some stage IA lung cancers are encouraging, a Japanese surgeon reported at the 3rd International Conference on Screening for Lung Cancer.
Junji Yoshida, MD, PhD, attending surgeon, Department of Thoracic Oncology, National Cancer Center Hospital East, Kashiwa, explained that the study, launched in 1998, is based on a system of lung cancer classification introduced by
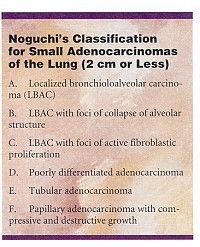
Masayuki Noguchi, MD, in 1995. Under this system, lung cancers 2 cm or smaller are classified into six types (see Table).
Carcinoma in Situ?
Based on histologic characteristics and prognosis, Dr. Noguchi concluded that type A, localized bronchioloalveolar carcinoma, and type B, localized bronchiolo-alveolar carcinoma with foci of collapse of alveolar structure, are carcinomas in situ. "If they are truly in situ carcinomas," Dr. Yoshida said, "limited resection is the management of choice for types A and B. As a result, at our institution, we are doing a clinical trial of limited resection for probable in situ adenocarcinoma in the lung periphery."
So far, 30 patients have been enrolled13 men and 17 women. The median age at enrollment was 64 years (range, 40 to 74 years). All patients accepted into the study must have high-resolution CT scans suggestive of a type A or B tumor. These scans, Dr. Yoshida noted, have ground-glass attenuation but no pleural indentations or vascular convergence.
Patients must be fit enough to undergo lobectomy and systematic lymph node dissection, since intraoperative findings may dictate such management. Patients with a history of malignancy within the past 5 years are excluded.
Noguchi’s classification is confirmed by intraoperative frozen section, Dr. Yoshida said. Performing such classification from a frozen section is difficult, he acknowledged, and takes about an hour.
EvG Staining
The researchers have found EvG staining to be "a great aid in distinguishing types A and B from type C tumors," he said. The EvG stain reveals whether elastic fibers in the alveolar wall are intact. If the elastic fibers are destroyed by tumor cells, the tumor is considered type C. Although still localized, type C bronchi-oloalveolar carcinomas have foci of active fibroblastic proliferation.
Diagnoses in the series include 1 type A tumor, 14 type B tumors, 3 cases of atypical adenomatous hyperplasia, 3 cases of fibrosis, and 1 granuloma. "In one case," Dr. Yoshida said, "frozen section diagnosis of type B was corrected to type C by postoperative pathologic study." Tumor diameters ranged from 5 mm to 2 cm, with a mean of 1.2 cm.
Wedge resections were performed in 20 patients, segmentectomies in 3, and lobectomy and lymph node dissection in 7. Video-assisted thoracic surgery utilizing three ports was used for 17 of the procedures, Dr. Yoshida noted. Resection margins of 1 cm are required for all type A and B tumors.
With no recurrences to date in the patients with malignant tumors, Dr. Yoshida is encouraged by the interim results. "With only 2 years of follow-up in this study," he said, "it is too early for strong conclusions, but Dr. Noguchi’s conclusions appear to be valid."