Low Dose Deferasirox Yields Promising Transfusion Independence in MDS
For patients with MDS who are relapsed/refractory to erythropoietin stimulating agents, low-dose deferasirox demonstrated promising efficacy and tolerability outcomes.
For patients with MDS who are relapsed/refractory to erythropoietin stimulating agents, low-dose deferasirox demonstrated promising efficacy and tolerability outcomes.
Results from the single-arm, multi-center, open-label phase 2 LODEFI study (NCT03387475) shared at the 2024 Hematology Annual Meeting & Exposition (ASH), showed that low-dose deferasirox (Jadenu) elicited promising transfusion independence (TI) and a favorable tolerance profile in patients with myelodysplastic syndrome (MDS) who are low-risk anemic.
At 12 months, a TI of 47.4% (95% CI, 31.0%-64.2%) was observed in patients treated with deferasirox. At a stricter definition of transfusion dependence, a burden of 4 or more red blood cell units every 8 weeks, 68.4% (95% CI, 51.3%-82.5%) of patients had an observed TI at 12 months.
Lead study author Sophie Park, MD, PhD, a professor at the Centre Hospitalier Universitaire de Grenoble, and coauthors wrote in the poster presented at ASH, “There is still an unmet medical need for patients with low-risk MDS who are refractory or relapsing to erythropoietin agents [ESAs] and transfusion dependent.” They also added, “Low dose deferasirox could be a potential treatment option for anemia in selected patients with MDS who are refractory or relapsing under ESA and with low transfusion burden.”
The study met its primary end point of efficiency of low-dose deferasirox on transfusion dependence at 12 months, defined by the need for 2 and more red blood cell units per 8 weeks for a total of 24 weeks between 6 and 12 months from the beginning of treatment. A key secondary end point replicated the primary one with more intensive requirements, as TI at 12 months was defined as a burden of more than 4 red blood cells units every 8 weeks for 24 weeks. The biological and clinical tolerability of low-dose deferasirox was also investigated.
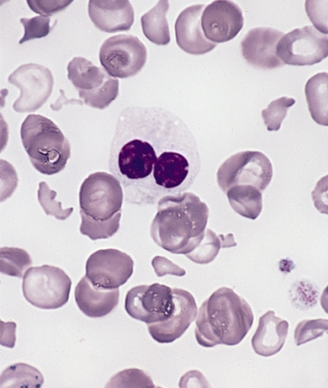
Patients with very low (n = 16), low (n = 19), and intermediate (n = 1) MDS based on Revised International Prognostic Scoring System and 2016 World Health Organization (WHO) Guidelines who are refractory or relapsing to ESAs, with low transfusion burden and a ferritin level under 1000 µg/l were enrolled into the trial.
Regarding dosage, all patients were given 3.5 mg/kg of deferasirox at inclusion to be taken orally every day for 12 months. At month 1, residual dosages of deferasirox were given to adapt the dosage at month 3 to reach approximately 3 µM. Prior to deferasirox, all patients had received ESA.
A total of 38 patients were enrolled; median age was 73.5 years (IQR, 69.0-78.0) and the median Charlson Comorbidity index was 4.0 (IQR, 3.0-5.0). Based on 2016 WHO guidelines, MDS subtypes included were MDS-single lineage dysplasia (SLD) (21.1%), MDS-multilineage dysplasia (MLD) (36.8%), MDS-RS (21.1%), chronic myelomonocytic leukemia (CMML)-1 (2.6%), MDS with excess blasts (MDS EB)-1 (7.9%), and unclassifiable MDS (MDS-U) (10.5%). The median ferritin level at inclusion was 547.0 µg/L (IQR, 399.0-849.0) and the median hemoglobin level was 86.0 g/L (IQR, 81.0-97.0). Additionally, 86.8% of patients were judged non-transfusion dependent (International Working Group 2018) and 13.2% were considered low transfusion burden.
According to the primary end point definition, MDS-RS had a lower rate of transfusion dependence than all other types of MDS, 28.6% vs 58.3%, respectively.
Regarding safety, low dose deferasirox was well-tolerated; renal and hepatic impairment led to treatment discontinuation and 1 diabetic patient overdosed on deferasirox. Adverse effects were mainly grade 1 to 3 of the digestive auditive renal variety.
Reference
Park S, Meunier M, Thepot S, et al. A phase 2 prospective study evaluating low-dose deferasirox in patients with low-risk myelodysplastic syndrome resistant or relapsing after erythropoietin stimulating agents (LODEFI). Blood. 2024;144(suppl 1):637. doi:10.1182/blood-2024-198104
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.