Maintenance Sunitinib Improved PFS in Extensive-Stage SCLC
In a phase II study, the use of maintenance sunitinib improved progression-free survival among patients with untreated extensive-stage small-cell lung cancer.
Maintenance sunitinib improved PFS in patients with SCLC
The use of maintenance sunitinib improved progression-free survival (PFS) over placebo among patients with untreated extensive-stage small-cell lung cancer (SCLC) in a new phase II study.
“Most of the 30,000 patients newly diagnosed each year with SCLC in the United States have extensive-stage disease,” wrote study authors led by Neal E. Ready, MD, PhD, of Duke University Medical Center in Durham, North Carolina. “Despite achieving good disease control initially, patients with SCLC usually experience relapse within 6 months of first-line chemotherapy and often do not respond to subsequent chemotherapy.”
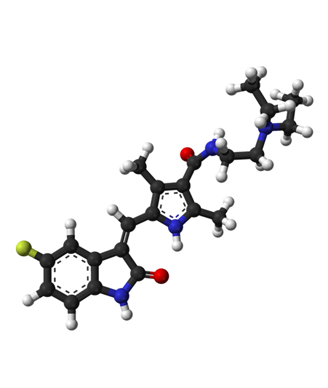
In previous studies, maintenance chemotherapy after standard platinum-based therapy did not show any overall survival benefit. The new study aimed to test whether sunitinib, a small-molecule tyrosine kinase inhibitor that inhibits VEGF receptors and other targets. Results of the new study were published online ahead of print in the Journal of Clinical Oncology.
The study enrolled a total of 144 patients, 49 of whom progressed or did not complete induction chemotherapy; 95 patients were randomly assigned to a placebo maintenance therapy group (46 patients) or a sunitinib maintenance therapy group (49 patients), and five patients on each arm did not receive the maintenance therapy. Sunitinib patients received 37.5 mg per day until progression.
The median PFS with sunitinib was 3.7 months, compared with 2.1 months with placebo, for a hazard ratio (HR) of 1.62 (95% CI, 1.02-2.60; P = .02). The median overall survival with sunitinib was 9 months, and 6.9 months with placebo, for an HR of 1.28 (95% CI, 0.79-2.10; P = .16). There were three complete responses during maintenance, all in the sunitinib group. Eighteen patients in the placebo group crossed over to sunitinib after progression, and 77% of those evaluable had stable disease for between 6 and 27 weeks.
In the sunitinib group, grade 3 adverse events included fatigue (19%), decreased neutrophils (7%), decreased leukocytes (7%), and decreased platelets (7%). In the placebo group, only fatigue (10%) occurred in more than 5% of the cohort. Grade 4 gastrointestinal hemorrhage occurred in one sunitinib patient, as did grade 4 pancreatitis, hypocalcemia, and elevated lipase in another. In the placebo group, one patient had grade 4 thrombocytopenia and one had grade 4 hypernatremia.
“The toxicity for sunitinib after standard chemotherapy may be greater in the setting of actively progressing SCLC compared with immediate maintenance therapy when the disease is stable,” the authors wrote. “These results support the future study of multitargeted VEGFR inhibitors in SCLC, especially as candidate predictive biomarkers are identified and in combination with new therapeutic strategies.”