Metastatic castration-resistant prostate cancer that is progressing despite docetaxel chemotherapy is difficult to treat and often aggressive. If not previously used, modern androgen signaling inhibitors have established clinical activity in this setting. Cabazitaxel and radium-223 have also been shown to extend survival in appropriately selected patients. Carboplatin-containing chemotherapy regimens have not been studied in randomized trials with a survival endpoint, but they have demonstrated activity in phase II trials and are occasionally considered in the post-docetaxel setting. Recent identification of potentially exploitable targets in the molecular makeup of advanced prostate cancer has created opportunities for clinical trials of novel targeted agents, with poly(ADP-ribose) polymerase inhibitors yielding compelling early results in molecularly selected patients. Much remains to be done to improve the lot of patients with docetaxel-unresponsive metastatic castration-resistant prostate cancer.
Metastatic castration-resistant prostate cancer that has become resistant to docetaxel chemotherapy represents one of the greatest clinical challenges in the management of this disease. Patients in this situation have an expected median survival that is typically less than 18 months, and they frequently suffer from symptoms related to progressive cancer and/or persistent treatment toxicity. More effective treatments for patients with taxane-resistant disease are desperately needed.
Standard Treatment Options
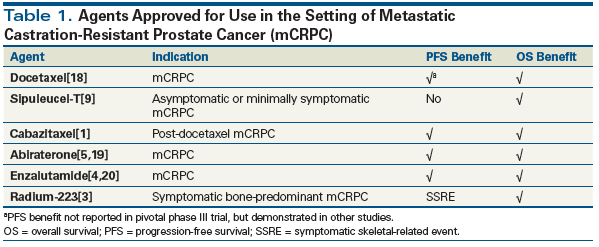
Six agents are approved for use in metastatic castration-resistant prostate cancer (Table 1), and several of these merit consideration in the post-docetaxel setting.
Cabazitaxel, which has been shown to improve overall survival (OS) and progression-free survival (PFS), was specifically studied in the post-docetaxel population, where it was compared (in conjunction with prednisone) with mitoxantrone plus prednisone.[1] Cabazitaxel is an appropriate choice regardless of distribution of disease. Recent studies demonstrate similar median survival for cabazitaxel administered at 20 mg/m2 and at 25 mg/m2; however, the lower dose often does not require growth factor support.[2]
Radium-223 was studied in patients with bone-predominant prostate cancer who were pretreated with chemotherapy or unfit for chemotherapy.[3] The median survival observed in that study (14.9 months for the radium-223 arm and 11.3 months for the control arm) reflects the advanced disease state of the patients treated in the ALSYMPCA trial. Because radium accumulates in the bones, the agent is only appropriate in patients without visceral disease and with lymph node metastases that are < 3 cm in size.
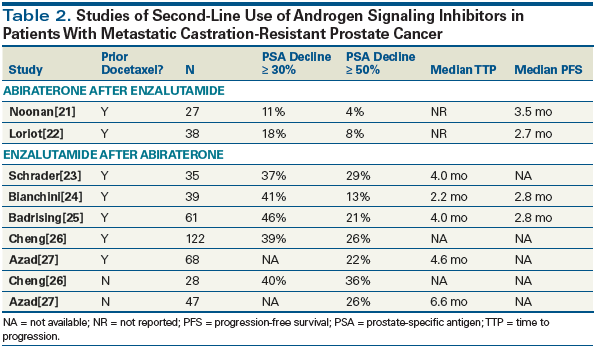
Both abiraterone and enzalutamide, the most potent inhibitors of androgen receptor signaling, were initially studied in docetaxel-pretreated patients. Both agents demonstrated OS and PFS improvements in that setting, as well as favorable differences in a variety of secondary measures of efficacy. Frequently, by the time advanced prostate cancer becomes resistant to docetaxel, patients will have been treated with one or even both of these androgen signaling inhibitors. If they have not, however, there is strong evidence for using at least one of these agents after docetaxel, based on the results of the AFFIRM study[4] and the COU-AA-301 study.[5] Whether both should be used is another matter altogether. There are no data regarding impact on survival of the second-line use of these agents, and small, often retrospective studies consistently show that the second-line use of androgen signaling inhibitors yields low response rates and disappointing response durations (Table 2). However, individual patients occasionally derive a clinical benefit from sequential use of these agents. Early data, which await validation, suggest that the detection of the alternative splice variant of the androgen receptor AR-V7 in circulating tumor cells may prove useful in identifying a proclivity for resistance to second-line androgen signaling inhibitor therapy, and if confirmed, could prove useful in determining which patients should get both agents and which should get only one.[6-8]
Although a small subset of patients enrolled in the pivotal clinical trial of sipuleucel-T[9] had been pretreated with docetaxel, a large majority of patients were chemotherapy-naive; therefore, there are few data to support the use of sipuleucel-T in docetaxel-resistant disease. It may be considered in unusual patients who are asymptomatic and have slowly progressing disease.
Other Chemotherapy Agents
A number of chemotherapy agents have been evaluated in prostate cancer. Mitoxantrone has largely been supplanted by cabazitaxel, as a result of the superiority of cabazitaxel in a head-to-head comparison of the two agents. The median PFS for mitoxantrone in the docetaxel-resistant population was only 1.4 months.[1] Thus, mitoxantrone is rarely used in docetaxel-resistant patients today.
Carboplatin has been known to have a modest level of activity in prostate cancer, as a single agent[10] and in a variety of combination regimens. For example, recent phase II studies reported activity for docetaxel plus carboplatin,[11] and for cabazitaxel plus carboplatin.[12] Carboplatin-containing regimens have been proposed for patients with so-called “aggressive variant prostate cancer,” a variably defined entity that generally presents as rapidly progressing metastatic prostate cancer with poorly differentiated histology, visceral involvement, and relatively low serum prostate-specific antigen (PSA) levels when measured against tumor burden.[13] Recent discoveries that DNA damage repair defects are more common than previously expected in advanced metastatic castration-resistant prostate cancer[14] may also provide a biologic explanation for why a minority of patients with advanced prostate cancer respond to carboplatin or carboplatin-containing regimens,[15] although there has not been a clinical trial to confirm an association between these genomic alterations and platinum sensitivity in advanced prostate cancer. Cisplatin and etoposide, standard agents for the treatment of small-cell prostate cancer (see following), have also been successfully employed in aggressive variant prostate cancer.[13]
Small-Cell Prostate Cancer
The discussion here is focused on the management of adenocarcinoma of the prostate. A rather rare phenomenon is the emergence of classic neuroendocrine small-cell prostate cancer. The diagnosis is classically made based on a biopsy in a patient who has rapidly evolving disease and often an undetectable or non-rising serum PSA level. Patients with classic small-cell prostate cancer are treated following protocols developed for small-cell carcinoma of the lung. While the overall prognosis in these patients is relatively poor, occasionally there are individuals who have durable chemotherapy responses.[16]
Precision Oncology
Finally, the characterization of the common genomic alterations in metastatic castration-resistant prostate cancer[14] has raised the possibility that targeted drugs that are not usually considered in prostate cancer may play a role in selected patients whose cancer harbors specific molecular alterations. Such an approach has not been validated and has not become standard of care, but a growing number of clinical trials are exploring it. At this stage, the rather striking activity of the poly(ADP-ribose) polymerase (PARP) inhibitor olaparib in patients whose tumors have specific DNA repair defects might justify the use of this agent in molecularly selected patients.[17] However, this approach awaits validation. Other potentially targetable defects are less common, and less is known about the promise of exploiting them. It is not yet clear whether tumor genotyping should be routinely recommended to all patients. At this point, such an approach has not been prospectively validated, and to date, results with PARP inhibitors are quite preliminary and require confirmation. Thus, routine genotyping of all patients is not currently standard practice. This is likely to evolve as data for molecularly selected therapies mature and expand.
KEY POINTS
- Docetaxel-resistant metastatic castration-resistant prostate cancer is challenging to treat and nearly universally fatal.
- Cabazitaxel, radium-223, enzalutamide, and abiraterone have demonstrated an overall survival benefit after docetaxel, and these agents can be considered in appropriately selected patients after docetaxel.
- Molecular characterization of individual cancers promises to make personalized therapy increasingly possible for patients with targetable molecular defects.
Another vexing issue is whether to recommend germline DNA testing for men with metastatic castration-resistant prostate cancer. This is an emerging area where the full implications of testing have yet to be clarified. A referral for genetic counseling should be considered, particularly in patients whose family members also have a history of cancer, but a routine practice standard remains to be established.
A Practical Approach
The general approach to a patient with docetaxel-resistant metastatic castration-resistant prostate cancer begins with an assessment of the patient’s health status, capacity to tolerate treatment, and goals of care, as well as the extent of disease, rate of progression, and symptom burden. A diagnostic biopsy is indicated when small-cell prostate cancer is suspected, since the treatment approach for this entity is distinct and affected patients may be considered for molecular analysis as part of a research program.
Assuming that the patient is fit for therapy and desires maximal care, consider treatment with an androgen signaling inhibitor if one has not been previously administered, then cabazitaxel, then radium-223. The order in which these agents might be offered is not well established, and the benefit of each line of therapy may diminish as the patient’s fitness for treatment declines. Some heavily pretreated patients with asymptomatic disease that is progressing slowly may benefit from observation alone, along with symptom-directed care as needed. In patients who clinically appear to have aggressive variant prostate cancer, a carboplatin/taxane combination can be considered. Symptom management and appropriate use of palliative radiation therapy, as well as supportive care interventions, are also important components of care. Referral for clinical trials, particularly those that include an analysis of the molecular makeup of the cancer, should be considered. Finally, if a patient is known to have DNA repair defects, the off-label use of a PARP inhibitor may be considered.
Financial Disclosure:Dr. Beer receives research funding from Astellas, Boehringer Ingelheim, Bristol-Myers Squibb, Dendreon, Janssen Research & Development, Medivation, OncoGenex, Sotio, and Theraclone Sciences/OncoResponse; he has consulted for AbbVie, AstraZeneca, Churchill Pharmaceuticals, Clovis Oncology, Dendreon, F. Hoffmann–La Roche Ltd, Janssen (Biotech, Oncology, and Research & Development), Janssen Japan, and Johnson & Johnson; and he holds stock in Salarium Pharmaceuticals.
References:
1. de Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147-54.
2. Sartor AO, Oudard S, Sengelov L, et al. Cabazitaxel vs docetaxel in chemotherapy-naive (CN) patients with metastatic castration-resistant prostate cancer (mCRPC): a three-arm phase III study (FIRSTANA). J Clin Oncol. 2016;34(suppl):abstr 5006.
3. Parker C, Nilsson S, Heinrich D, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213-23.
4. Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187-97.
5. de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995-2005.
6. Antonarakis ES, Lu C, Wang H, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028-38.
7. Antonarakis ES, Lu C, Luber B, et al. Androgen receptor splice variant 7 and efficacy of taxane chemotherapy in patients with metastatic castration-resistant prostate cancer. JAMA Oncol. 2015;1:582-91.
8. Scher HI, Graf RP, Schreiber NA, et al. Nuclear-specific AR-V7 protein localization is necessary to guide treatment selection in metastatic castration-resistant prostate cancer. Eur Urol. 2017;71:874-82.
9. Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411-22.
10. Jungi WF, Bernhard J, Hurny C, et al. Effect of carboplatin on response and palliation in hormone-refractory prostate cancer. Swiss Group for Clinical Cancer Research (SAKK). Support Care Cancer. 1998;6:462-8.
11. Ross RW, Beer TM, Jacobus S, et al. A phase 2 study of carboplatin plus docetaxel in men with metastatic hormone-refractory prostate cancer who are refractory to docetaxel. Cancer. 2008;112:521-6.
12. Bilen MA, Cauley DH, Atkinson BJ, et al. Safety of same-day pegfilgrastim administration in metastatic castration-resistant prostate cancer treated with cabazitaxel with or without carboplatin. Clin Genitourin Cancer. 2017;15:e429-e435.
13. Aparicio AM, Harzstark AL, Corn PG, et al. Platinum-based chemotherapy for variant castrate-resistant prostate cancer. Clin Cancer Res. 2013;19:3621-30.
14. Robinson D, Van Allen EM, Wu YM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161:1215-28.
15. Hager S, Ackermann CJ, Joerger M, et al. Anti-tumour activity of platinum compounds in advanced prostate cancer-a systematic literature review. Ann Oncol. 2016;27:975-84.
16. Ciszewski A, Shackleton D, Beer TM. Long-term remission of metastatic small cell carcinoma of the prostate. Urology. 2008;71:546.e3-e4.
17. Mateo J, Carreira S, Sandhu S, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373:1697-708.
18. Tannock IF, de Wit R, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502-12.
19. Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138-48.
20. Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424-33.
21. Noonan KL, North S, Bitting RL, et al. Clinical activity of abiraterone acetate in patients with metastatic castration-resistant prostate cancer progressing after enzalutamide. Ann Oncol. 2013;24:1802-7.
22. Loriot Y, Bianchini D, Ileana E, et al. Antitumour activity of abiraterone acetate against metastatic castration-resistant prostate cancer progressing after docetaxel and enzalutamide (MDV3100). Ann Oncol. 2013;24:1807-12.
23. Schrader AJ, Boegemann M, Ohlmann CH, et al. Enzalutamide in castration-resistant prostate cancer patients progressing after docetaxel and abiraterone. Eur Urol. 2014;65:30-6.
24. Bianchini D, Lorente D, Rodriguez-Vida A, et al. Antitumour activity of enzalutamide (MDV3100) in patients with metastatic castration-resistant prostate cancer (CRPC) pre-treated with docetaxel and abiraterone. Eur J Cancer. 2014;50:78-84.
25. Badrising S, van der Noort V, van Oort IM, et al. Clinical activity and tolerability of enzalutamide (MDV3100) in patients with metastatic, castration-resistant prostate cancer who progress after docetaxel and abiraterone treatment. Cancer. 2014;120:968-75.
26. Cheng HH, Nadal R, Gulati R, et al. The effect of prior abiraterone (Abi) use on the activity of enzalutamide (Enza) in men with mCRPC. J Clin Oncol. 2014;32(suppl):abstr 18.
27. Azad AA, Eigl BJ, Murray RN, et al. Efficacy of enzalutamide following abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer patients. Eur Urol. 2015;67:23-9.