Melanoma Risk Genetic Testing May Help With Prevention
Positive genetic risk information about melanoma may help to prompt people to discuss melanoma risk with a wider variety of family members, according to a new study.
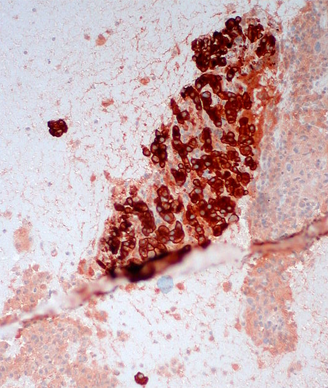
Malignant melanoma, liver FNA; source: Ed Uthman, Wikimedia Commons
Positive genetic risk information about melanoma may help to prompt people to discuss melanoma risk with a wider variety of family members, according to a study published in JAMA that examined the effects of hypothetical genetic testing. Interestingly, even people who received negative genetic testing results were still affected by the results.
“This study shows us that individuals are sensitive to receiving genetic risk information, regardless of the results, and will likely increase their willingness to discuss melanoma risk and prevention strategies with their families after receiving this type of feedback,” said study author Mallorie Gordon, MA, of the department of psychology, New School for Social Research, New York, New York.
“This study indicates that providing genetic risk information to patients and their families may not only improve their understanding of their particular skin health needs-specifically telling patients whether their melanoma risk is related to heredity or sun exposure, as defined by the feedback type of the genetic test-but also improve the risk communication that exists around melanoma and its prevention overall,” she told Cancer Network.
In the study, Gordon and colleagues randomly assigned 139 participants with first-degree relatives with melanoma to receive one of six feedback scenario conditions. Feedback could include information on inherited mutations in CDKN2A linked to heredity melanoma, on MC1R, which interacts with sun exposure to heighten population melanoma risk, and on nongenetic risk that incorporated factors like number of moles. Risk levels were either positive (higher risk) or negative. In addition, all participants were reminded of their increased risk due to family history regardless of the test findings.
The researchers asked participants at baseline about family discussions of melanoma risk, including how much they talked about risk to various members of their family. At follow-up, the researchers asked about participants’ intention to speak with these same family members about melanoma risk.
“This study found that genetic testing increased intended risk discussion with multiple family members, including parents, siblings, and children,” Gordon said. “In particular, receiving positive genetic risk information-meaning that the genetic testing showed that the individual was at increased risk for developing melanoma-would lead to a larger intended increase in family risk discussion than when receiving negative results.”
Results showed that melanoma risk discussions occurred more often on average, among women than men. However, the frequency of risk discussions did not vary by the number of first-degree relatives with melanoma or whether they had a sun-sensitive phenotype or not. People were more likely to indicate intent to have a discussion about risk if they received positive compared with negative feedback.
“Participants were especially likely to increase their discussions of melanoma risk with their siblings and their children, regardless of the results of their genetic testing feedback,” Gordon said. “While discussions around risk were already high and tended to stay that way with parents (both mothers and fathers), intended discussion with sisters, brothers, and children increased even more when genetic risk information was conveyed.”
Based on the results of this study, the researchers felt that genetic test findings may lead people to move beyond their typical communication patterns to discuss salient cancer risk information.