Mesotheliomas Associated With Lymphoma Radiation Therapy Feature Unusual Characteristics
Mesotheliomas that arise after patients receive radiation therapy for lymphoma have unusual histologic features, and those patients tend to be younger and tend to survive longer than more common asbestos-related mesothelioma patients.
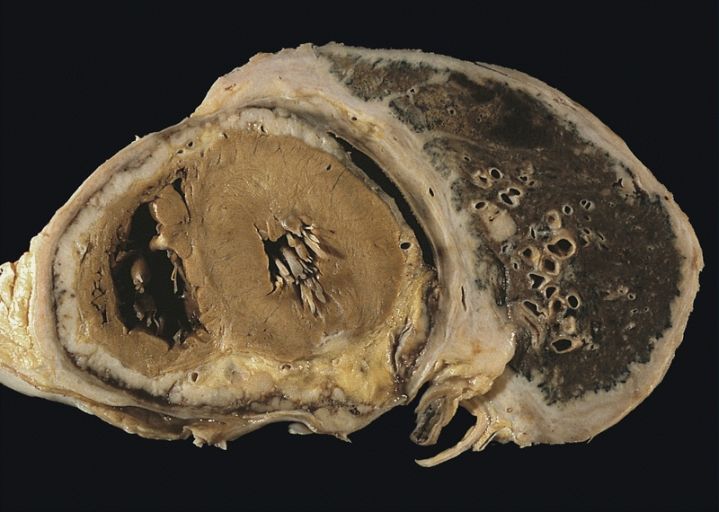
Diffuse pleural mesothelioma with extensive involvement of the pericardium
Mesotheliomas that arise after patients receive radiation therapy for lymphoma have unusual histologic features, and those patients tend to be younger and tend to survive longer than more common asbestos-related mesothelioma patients, according to a new study.
Pleural diffuse malignant mesothelioma (PDMM) are most commonly associated with asbestos, but other causes have recently been identified; among those is radiation treatment for other malignancies, including lymphoma, breast cancer, lung cancer, and others. “Patients with Hodgkin lymphoma have a 20-fold increased risk of mesothelioma after radiotherapy,” wrote researchers led by Lucian R. Chirieac, MD, of Brigham and Women’s Hospital in Boston. Chirieac and colleagues studied 1,618 consecutive patients with PDMM in order to better characterize the tumors associated with radiation for Hodgkin and non-Hodgkin lymphoma. The study’s results were published online ahead of print in November in the Journal of Clinical Oncology.
Among that overall cohort, the investigators identified only 22 patients who developed PDMM following chest radiation as part of lymphoma treatment. The mean latency time from radiation therapy to diagnosis of mesothelioma was 21.4 years; 20 of the 22 received radiation therapy for Hodgkin lymphoma.
Several differences were evident between the PDMM associated with lymphoma radiation and those associated with asbestos. The lymphoma-associated patients were younger, with a mean age of 46.7 years, compared with 63.3 years for asbestos-related patients (P < .001). Asbestos bodies were also substantially higher in the latter group, at a median of 325 bodies/g compared with only 15 bodies/g for the lymphoma-associated patients (P < .001). That was similar to a control group without PDMM (10 bodies/g).
A higher percentage of lymphoma-related PDMM patients had epithelioid histology, though this did not reach significance (77.3% vs 60.9%; P = .21). The authors noted that two lymphoma-associated PDMM cases demonstrated an unusual histology involving rhabdoid cells with high-grade cytology and cellular pleomorphism.
The median overall survival time was significantly better among lymphoma-associated PDMM patients, at 32.5 months vs 12.7 months (P = .018). An adjusted analysis showed that female sex, younger age, and epithelioid histology were favorable predictors of survival.
“These findings most likely reflect the complexity of this extremely unusual type of malignant neoplasm,” the authors concluded. “Mechanistic explanations for these associations are needed to improve our understanding of tumor morphogenesis and to help with the diagnostic recognition of tumors that have developed along various molecular pathways. Such diagnostic advances would likely have subsequent implications for patient management.”