Correct Answers:
1: C2: C
A 44-year-old patient with a history of stage IIB colorectal cancer at the hepatic flexure, invading the duodenum and pancreas, was initially diagnosed in September 2005 and received modified Whipple surgery and 8 cycles of adjuvant chemotherapy with capecitabine and oxaliplatin every 3 weeks.
Oncology (Williston Park). 30(11):992–994, 1000–1001.

Figure 1. Patient’s Platelet Counts
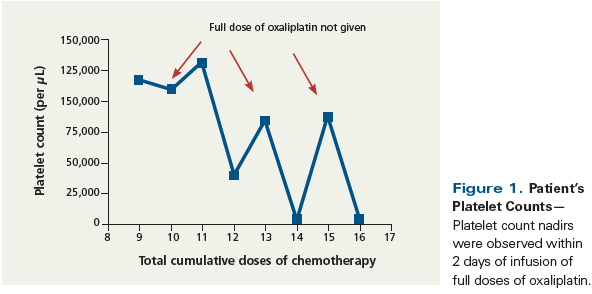
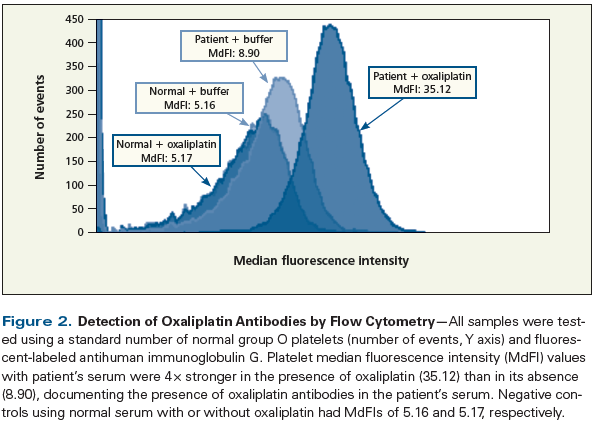
Figure 2. Detection of Oxaliplatin Antibodies by Flow Cytometry
A 44-year-old patient with a history of stage IIB colorectal cancer at the hepatic flexure, invading the duodenum and pancreas, was initially diagnosed in September 2005 and received modified Whipple surgery and 8 cycles of adjuvant chemotherapy with capecitabine and oxaliplatin every 3 weeks. His cancer was characterized by high microsatellite instability and was found to be related to underlying hereditary nonpolyposis colorectal cancer. He remained in complete remission until April 2015, when he was diagnosed with a second primary-stage IV colorectal adenocarcinoma. In June, he was started on a palliative chemotherapy regimen in which cycle 1 consisted of fluorouracil (5-FU) and oxaliplatin (for a total of 9 cumulative doses of oxaliplatin), which had to be dose-reduced by 20% due to hyperbilirubinemia secondary to underlying liver disease thought to be related to nonalcoholic steatohepatitis. In cycle 2, oxaliplatin was not given because of worsening hyperbilirubinemia (this would have been his 10th oxaliplatin dose). Cycles 3 (scheduled oxaliplatin dose #11) and 4 (scheduled oxaliplatin dose #12) were given without major complications, but a platelet count drop from 135,000/μL to 39,000/μL was noted 2 days after infusion in cycle 4. For cycle 5 (scheduled oxaliplatin dose #13), oxaliplatin was held due to thrombocytopenia of 77,000/μL, and only 5-FU was given. On day 2 of cycle 6 (scheduled oxaliplatin dose #14), a profound acute thrombocytopenia was noted, with a platelet count drop from 89,000/μL to 5,000/μL, although without any additional symptoms. Immediately following a platelet transfusion, the patient’s platelet count increased to 13,000/μL, which represented an inappropriately small increase in count. However, the platelet count later returned to the patient’s baseline (~89,000/μL). Cycle 7 (scheduled oxaliplatin dose #15) was delayed because of neutropenia (absolute neutrophil count, 800/μL). After reintroduction of oxaliplatin for cycle 8 (scheduled oxaliplatin dose #16), the patient’s platelet count dropped from 89,000/μL to 1,000/μL within 6 hours, this time accompanied by acute gastrointestinal hemorrhage. The pattern of the patient’s recurrent thrombocytopenia in relation to the timing of the scheduled chemotherapy is shown in Figure 1. Since he was receiving 5-FU at the time of these events (it was given approximately 6 hours after the oxaliplatin dose), the infusion with 5-FU was stopped. He was given 15 mg of intravenous dexamethasone and 2 units of platelet apheresis products and was admitted to the hospital for further management. His platelet count improved suboptimally to 12,000/μL after platelet transfusions, and the gastrointestinal hemorrhage stopped soon thereafter. The platelet count stabilized at 20,000/μL to 30,000/μL for the following 2 days, without additional platelet transfusions. Treatment with oral prednisone, 1 mg/kg, was continued for 2 more days. His platelet count further improved, up to 101,000/μL.
A. Direct antiglobulin test (DAT).
B. Bone marrow biopsy.
C. Flow cytometry for oxaliplatin-dependent platelet antibodies.
D. Peripheral blood smear.
E. Enzyme-linked immunosorbent assay (ELISA) for heparin-induced thrombocytopenia (HIT) antibodies.
A. Steroids.
B. Intravenous immunoglobulin (IVIG).
C. Discontinuation of the suspected drug.
D. Plasmapheresis.
E. Platelet transfusion.
Drug-dependent acute thrombocytopenias are rare cases of acute immune-mediated depletion of platelets. They are serious events that often are not identified as having been triggered by a causative drug. They can be induced by a variety of medications, including antibiotics and chemotherapeutic agents. Oxaliplatin is a drug that is commonly used to treat malignancies of the gastrointestinal tract; it is usually used in combination with 5-FU or irinotecan to treat colorectal adenocarcinoma. As with other chemotherapeutics, myelosuppression is a common side effect of oxaliplatin that can result in a combination of neutropenia, anemia, and thrombocytopenia. Less frequently, oxaliplatin can cause a drug-dependent acute thrombocytopenia as a result of sudden immune-mediated platelet destruction.
The commonly used criteria for predicting the presence of drug-dependent platelet antibodies are:
1) The patient was exposed to the suspected offending drug prior to onset of thrombocytopenia.
2) Normalization of the platelet count is seen after discontinuation of the suspected offending drug.
3) The suspected drug was the only drug that was used.
4) Other drugs were reintroduced or continued without causing acute thrombocytopenia.
5) Other causes of thrombocytopenia have been excluded.
6) Re-exposure to the offending drug caused thrombocytopenia.[1]
1: C2: C
The standard test for confirming the presence of oxaliplatin-dependent immunoglobulin G (IgG) platelet antibodies is flow cytometry,[2] which is performed on the patient’s serum in both the presence and absence of oxaliplatin, using fluorescent-labeled antihuman IgG that is able to detect platelet-bound drug-dependent IgG antibodies (Question 1, Answer C). Typically, thrombocytopenia that develops as a result of bone marrow suppression after oxaliplatin has a platelet count nadir approximately 7 to 14 days after administration of the drug. Oxaliplatin-dependent immune-mediated acute thrombocytopenia results in a sudden depletion of platelets immediately after exposure to the offending drug if the drug-dependent IgG antibody is present in the patient’s blood.[3] The condition may be difficult to diagnose unless a platelet count is performed in a timely manner, soon after administration of the causative agent-either when the mediating drug is still active or while the patient is still recovering from the acute thrombocytopenia.
Hemolysis and neutropenia, as well as systemic reactions such as fever and chills, can be part of the clinical presentation. Antibodies to neutrophils, red blood cells, and platelets can be present concurrently.[4] Our patient did not display signs of hemolysis or neutropenia, nor did he develop a systemic reaction; therefore, there was no reason to test for red blood cell destruction, making Answer A to Question 1 incorrect. His haptoglobin and lactate dehydrogenase levels, and the results of his DAT, remained within normal limits and no leukopenia was observed. Since this patient had isolated acute thrombocytopenia that presented in a pattern related to the administration of oxaliplatin, and given that no other potential causes were detected, a bone marrow biopsy (Question 1, Answer B) is not indicated.[5]
A peripheral blood smear is always indicated in patients with new onset of thrombocytopenia. It is important for ruling out thrombotic thrombocytopenic purpura (TTP), which requires inspection of the peripheral blood smear for schistocytes. Our patient did not present with symptoms consistent with TTP (no evidence of altered mental status; fever; impaired organ function, including renal and hepatic function; or diarrhea). Furthermore, no schistocytes were detected. Even though a peripheral blood smear (Question 1, Answer D) is crucial to obtain in this patient,[6] it is not the best single test for verifying the diagnosis.
Our patient has frequently been exposed to heparin, given that he has received his chemotherapy treatments through a port, which has regularly been flushed with heparin to prevent occlusion by clots. A 4T score of 4 showed an intermediate predicted probability of the presence of HIT antibodies. An HIT ELISA is recommended in this setting,[7] even though the pattern of the patient’s thrombocytopenia makes HIT an unlikely cause of his low platelet count. A negative result on HIT ELISA would not explain the patient’s low platelet count; a positive test would require a confirmatory test (serotonin release assay). Thus, in this setting, an HIT ELISA (Question 1, Answer E) is a reasonable test to obtain, but it is not the best single test to order.
The clinical picture is strongly suggestive of the presence of oxaliplatin-dependent platelet antibodies; therefore, cessation of the drug as the suspected offender is the best management option (Question 2, Answer C). Removal of the offending agent from a patient’s blood typically results in rapid and sustained recovery of the platelet count. Whether there is additional clinical benefit from the use of steroids or IVIG remains questionable. A large case series favors cessation of the drug rather than use of steroids or IVIG in the setting of drug-dependent platelet antibody–induced thrombocytopenia.[8] Therefore, Answers A and B are both incorrect for Question 2.
Drug-dependent IgG platelet antibodies are difficult to remove with plasmapheresis, as has been noted in case reports that examined the optional use of plasmapheresis in patients with HIT antibodies; moreover, a fast rebound of IgG is expected on removal of the offending agent.[9] Plasmapheresis (Question 2, Answer D) remains a potentially useful tool in the setting of uncontrolled acute bleeding, where rapid removal of antibodies is required. Nonetheless, it is not the best management for drug-dependent platelet antibody–induced thrombocytopenia.
Platelet transfusion is a useful tool for increasing the platelet count in a clinical setting in which increased nonimmunologically driven platelet consumption or wasting is the primary mechanism of the thrombocytopenia, and where replacement is needed to prevent bleeding. As demonstrated in this case, despite transfusion of platelets, the platelet count only increased marginally. The transfusion of platelets (Question 2, Answer E) remains a useful tool to potentially help a patient in the setting of an acute hemorrhage, but it is not the best management option in our patient, since transfused platelets usually will also be destroyed and removed by the circulating drug-dependent IgG antibodies as long as the drug remains in the patient’s blood.
Results of the patient’s flow cytometry were positive and confirmed the presence of oxaliplatin-dependent IgG platelet antibodies (Figure 2). The patient completely recovered from his thrombocytopenia, and his treatment for colorectal cancer was modified to 5-FU monotherapy. Oxaliplatin was not reintroduced to his treatment plan again, and he did well, with no reoccurrence of severe acute thrombocytopenia.
Usually at least 10 doses of oxaliplatin must be given before thrombocytopenia develops in a susceptible patient, and reviews of the literature suggest that patients receive an average of 16.8 doses before development of oxaliplatin-related thrombocytopenia.[10,11] A case series concluded that the onset of acute thrombocytopenia usually starts as early as during the administration of the offending drug or 1 day after administration of the dose is complete.[12] Rapid recovery is commonly seen; therefore, a high number of missed cases seems likely. Our patient was diagnosed with drug-dependent platelet antibodies after he had two episodes of thrombocytopenia that were more profound than would normally have been expected. Sensitivity to the offending drug usually persists indefinitely,[13] and rechallenge with oxaliplatin is likely to result in a recurrence of drug-induced thrombocytopenia. Nonetheless, a correct diagnosis and appropriate management remain challenges for the physician and the patient. With regard to treatment, cessation of the offending drug is the gold standard, and neither IVIG nor steroids may have any additional benefit in drug-induced thrombocytopenia.[8] Although drug-induced thrombocytopenia is often suspected, case reports are limited. We would encourage clinicians to regularly use the criteria listed at the beginning of this discussion to predict the presence of drug-dependent platelet antibodies, in a manner similar to that in which the 4T score is used to predict the likelihood of HIT. This would help improve the rate of accurate diagnosis and help patients receive appropriate management.
Financial Disclosure:The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
E. David Crawford, MD, serves as Series Editor for Clinical Quandaries. Dr. Crawford is Professor of Surgery, Urology, and Radiation Oncology, and Head of the Section of Urologic Oncology at the University of Colorado School of Medicine; Chairman of the Prostate Conditions Education Council; and a member of ONCOLOGY's Editorial Board.
If you have a case that you feel has particular educational value, illustrating important points in diagnosis or treatment, you may send the concept to Dr. Crawford at david.crawford@ucdenver.edu for consideration for a future installment of Clinical Quandaries.
1. Curtis BR. Drug-induced immune thrombocytopenia: incidence, clinical features, laboratory testing, and pathogenic mechanisms. Immunohematology. 2014;30:55-65.
2. Visentin GP, Wolfmeyer K, Newman PJ, Aster RH. Detection of drug-dependent, platelet-reactive antibodies by antigen-capture ELISA and flow cytometry. Transfusion. 1990;30:694-700.
3. Aster RH. Drug-induced immune thrombocytopenia: an overview of pathogenesis. Semin Hematol. 1999;36:2-6.
4. Fontao-Wendel R, Hoff PM, Lazar A, et al. Immune-mediated pancytopenia induced by oxaliplatin: a case report. Transfusion. 2010;50: 1453-9.
5. Jones EC, Boyko WJ. Diagnostic value of bone marrow examination in isolated thrombocytopenia. Am J Clin Pathol. 1985;84:665-7.
6. Bain BJ. Diagnosis from the blood smear. N Engl J Med. 2005;353: 498-507.
7. Lo GK, Juhl D, Warkentin TE, et al. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4:759-65.
8. Pedersen-Bjergaard U, Andersen M, Hansen PB. Drug-induced thrombocytopenia: clinical data on 309 cases and the effect of corticosteroid therapy. Eur J Clin Pharmacol. 1997;52:183-9.
9. Warkentin TE, Sheppard JA, Chu FV, et al. Plasma exchange to remove HIT antibodies: dissociation between enzyme-immunoassay and platelet activation test reactivities. Blood. 2015;125:195-8.
10. Suzuki K, Oda H, Sugawara Y, et al. Oxaliplatin-induced acute thrombocytopenia: a case report and review of the literature. Intern Med. 2013;52:611-5.
11. Ohta S, Cho Y, Oshima S, et al. Oxaliplatin-induced acute-onset thrombocytopenia and hemorrhage: case report and review of the literature. Oncol Lett. 2012;3:1297-300.
12. Forcello NP, Khubchandani S, Patel SJ, Brahaj D. Oxaliplatin-induced immune-mediated cytopenias: a case report and literature review. J Oncol Pharm Pract. 2015;21:148-56.
13. Curtis BR, Kaliszewski J, Marques MB, et al. Immune-mediated thrombocytopenia resulting from sensitivity to oxaliplatin. Am J Hematol. 2006;81:193-8.