Mitomycin Exhibits Durable Responses in Recurrent, Low-Grade NMIBC
Adverse reactions in the phase 3 ENVISION trial were largely mild to moderate in severity, and serious reactions occurred in 12% of those with NMIBC.
Efficacy data from the phase 3 ENVISION trial revealed that the 24-month duration of response rate was 72.2% by Kaplan Meier estimation.
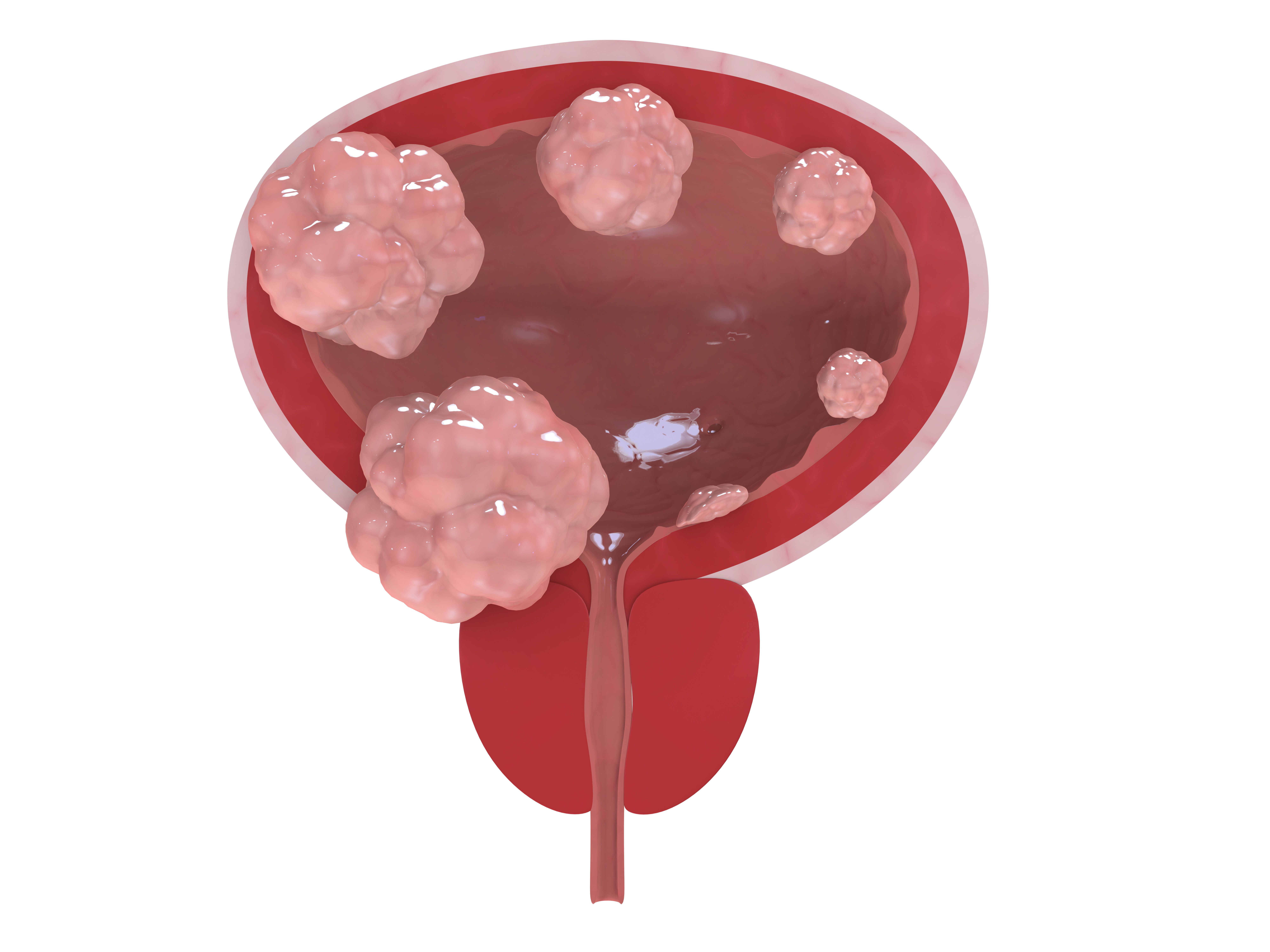
Mitomycin (Zusduri) exhibited durable responses in patients with recurrent, low-grade, intermediate-risk non–muscle-invasive bladder cancer (LG-IR-NMIBC), according to a news release from the drug’s developer, UroGen Pharma.1
Efficacy data from the phase 3 ENVISION trial (NCT05243550) revealed that the 24-month duration of response (DOR) rate was 72.2% (95% CI, 64.1%-78.8%) by Kaplan Meier estimation. This was achieved among patients who attained a complete response (CR) at 3 months (79.6%). Additional data revealed that the median DOR was not reached, and the median follow-up time after 3-month CR was 23.7 months.
Regarding safety, adverse reactions (ARs) were largely mild to moderate in severity, with 12% of patients experiencing serious ARs. ARs occurring in at least 10% of patients included dysuria, increased potassium, increased creatinine, decreased hemoglobin, increased eosinophils, increased aspartate aminotransferase, increased alanine aminotransferase, decreased lymphocytes, urinary tract infection, decreased neutrophils, and hematuria. Furthermore, serious urinary retention and urethral stenosis occurred in 0.8% and 0.4% of patients, respectively.
“This latest update from the pivotal ENVISION trial of [mitomycin] showed that, among patients who achieved a CR at 3 months, the probability of remaining event-free 24 months after CR was 72.2%,” Sandip Prasad, MD, MPhil, director of Genitourinary Surgical Oncology and vice chair of Urology at Morristown Medical Center/Atlantic Health System, and principal investigator of the ENVISION trial, said in the news release.1 “Among patients who achieved a CR, the event rate over time has remained stable.”
Patients in the phase 3 single-arm study (n = 240) received 6 weekly intravesical injections of mitomycin at 75 mg in the ambulatory setting.2 Patients were assessed via cystoscopy, urine cytology, and for-cause biopsy for response, with those having no evidence of disease designated as having a CR and those with evidence of disease as a non-CR. Patients with a CR entered quarterly follow-up, and those without were treated according to standard of care during follow-up.
Those with positive or suspicious cytology were evaluated excluding upper tract urothelial carcinoma and underwent bladder biopsies if negative. Patients with negative evaluations on bladder biopsies were classified as having a CR.
Patients in the phase 3 trial had a median age of 70.0 years (range, 30-92) and were mostly male (61%) and White (98%). The most common countries of enrollment included Bulgaria (35%), the US (17%), and Latvia (16%). Patients most commonly had an American Society of Anesthesiologists (ASA) status of II (52%), defined as mild systemic disease, and most patients (53%) had a history of smoking.
A total of 95% of patients underwent all 6 treatment instillations, and 83% had multiple tumors. Furthermore, 52% of patients had a previous NMIBC episode within a year of current diagnosis, 60% had 1 previous NMIBC episode, and 63% received 1 transurethral resection of bladder tumors. Additionally, 5.8% received prior Bacillus Calmette-Guérin treatment, 23% received prior intravesical chemotherapy, and 10% received prior mitomycin.
The primary end point of the study was the 3-month CR rate. DOR and safety were secondary outcomes.
“This DOR result highlights the sustained efficacy of the therapy and reinforces its potential as a durable treatment option. For the first time, adult patients with recurrent LG-IR-NMIBC have an FDA-approved therapy,” Prasad concluded.1 “This marks a potentially transformative step forward in how we manage this chronic, highly recurrent, and disruptive cancer. [Mitomycin] is a new, outpatient treatment option for patients that can help provide a clinically meaningful recurrence-free interval, which is compelling given the highly recurrent nature of LG-IR-NMIBC.”
References
- UroGen announces 24-month duration of response of 72.2% from the pivotal phase 3 ENVISION trial of ZUSDURI, the first and only FDA-Approved medicine for recurrent low-grade intermediate-risk non-muscle invasive bladder cancer. News release. UroGen Pharma. August 5, 2025. Accessed August 6, 2025. https://tinyurl.com/4p6mrkhy
- Prasad SM, Shishkov D, Mihaylov NV, et al. Primary chemoablation of recurrent low-grade intermediate-risk nonmuscle-invasive bladder cancer with UGN-102: a single-arm, open-label, phase 3 trial (ENVISION). J Urol. 2025;213(2):205-216. doi:10.1097/JU.0000000000004296