Mixed-Beam Radiation Therapy Can Cut Total Radiation Dose
BOSTON-An experimental mixed-beam radiation technique can reduce the total radiation dose required by a factor of two in simple cancer cases, Michelle M. Svatos, PhD, reported at the American Society for Therapeutic Radiology and Oncology (ASTRO) annual meeting.
BOSTONAn experimental mixed-beam radiation technique can reduce the total radiation dose required by a factor of two in simple cancer cases, Michelle M. Svatos, PhD, reported at the American Society for Therapeutic Radiology and Oncology (ASTRO) annual meeting.
The technique adds an electron field to the typical photon mix for intensity modulated radiation therapy (IMRT). As a result, the dose is distributed in a way that delivers more radiation to the tumor and less to healthy tissue in extraneous areas.
"This is a new way of using existing technology," Dr. Svatos, a medical physicist at Siemens Oncology Care Systems, Con-cord, California, told ONI after her talk. She said that patients should be able to tolerate it better with fewer side effects.
Dr. Svatos demonstrated its potential by showing a mixed-beam IMRT treatment plan for a large lymphoepithelioma of the maxillary sinus (see Figure) treated at the University of California, San Francisco, where she was a postdoctoral fellow before joining Siemens.
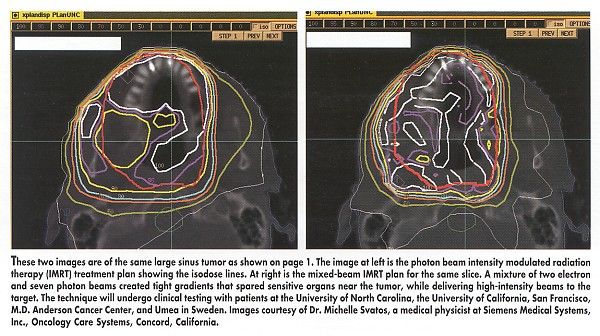
A mixture of two electron and seven photon beams created tight gradients that spared sensitive organs near the tumor, while delivering high-intensity beams to the target. As a result, there was a 20% savings overall in extraneous dose to normal tissue, she said.
The electron beam need not fully cover the target at depth, Dr. Svatos and her colleagues concluded, because the photon beams can "fill in" to make the tumor dose homogenous.
Adding a single electron field will often be enough to produce a reduced integral dose, they reported.
Dr. Svatos developed the technique in collaboration with Dr. Julian Rosenman, of the University of North Carolina, Chapel Hill, where they used a standard Siemens MD linear accelerator that was in clinical use. They constructed mathematically spherical tumors with radii varying from 1 to 6 cm and optimized treatments plans with PlanUNC (University of North Carolina) treatment planning software.
Mixing beams is not a new idea, Dr. Svatos said, but recent tools have made better dose calculation and inverse planning possible. Instead of the technician figuring out how to deliver the dose, the computer calculates the distribution.
The researchers plan to test the technique with patients at the University of North Carolina, University of California, San Francisco, M.D. Anderson Cancer Center, and Umea in Sweden. Dr. Svatos said she hoped to be able to announce results at next year’s ASTRO meeting.