Monoclonal Antibody Effective in Refractory Myeloma
Daratumumab, a monoclonal antibody that targets CD38, was safe and effective in patients with heavily pretreated and refractory multiple myeloma.
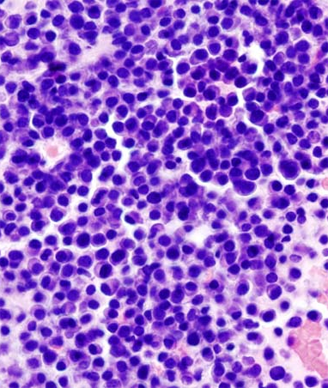
Micrograph showing multiple myeloma. Copyright © KGH.
Daratumumab, a monoclonal antibody that targets CD38, was safe and effective in patients with heavily pretreated and refractory multiple myeloma, according to the results of a study published in the New England Journal of Medicine. CD38 is highly and uniformly expressed on myeloma cells.
“Daratumumab monotherapy (at a dose of 16 mg per kilogram) induced durable responses that deepened over time, including complete and very good partial responses, with 65% of the patients who had a response remaining progression-free at 12 months,” wrote researchers led by Henk M. Lokhorst, MD, PhD, of the VU University Medical Center in Amsterdam. “The responses compare favorably with those observed with other investigational agents in patients with relapsed myeloma or relapsed and refractory myeloma.”
In an editorial published with the study, Noopur Raje, MD, and Dan L. Longo, MD, from the Massachusetts General Hospital Cancer Center and Harvard Medical School, called the introduction of an effective monoclonal antibody into the treatment of myeloma “game changing.”
“These agents have the advantage of an immune-based approach without the need for patient-specific cell manipulation. Their limited toxicity allows for easy combining with existing therapies,” they wrote.
The study looked at daratumumab in two parts: part 1 was a dose-escalating study and part 2 was a dose-expansion phase.
Part 1 of the study looked at daratumumab from doses of 0.005 to 24 mg/kg of body weight; no maximum tolerated dose was identified.
In part 2 of the study, the researchers assigned 30 patients to 8 mg/kg of daratumumab and 42 patients to 16 mg/kg. Doses were administered once weekly for eight doses, twice monthly for eight doses, and monthly for up to 2 years. Patients included in the analysis had a median of four prior treatments. About 80% of patients were refractory to the last therapy they received and 76% had undergone autologous stem-cell transplantation.
The overall response rate to the treatment was 36% for patients assigned the 16-mg dose with 15 patients having a partial response or better and two patients with a complete response. The overall response rate was 10% among patients assigned the 8 mg/kg dose.
For 16-mg daratumumab, the median progression-free survival was 5.6 months (95% confidence interval [CI], 4.2–8.1), and 65% of patients who had a response were progression-free at 1 year.
Overall, reactions related to drug infusion were mild and no dose-dependent adverse reactions occurred. The most common grade 3/4 adverse reactions were pneumonia and thrombocytopenia.
Commenting on these positive results, Raje and Longo also cautioned that there remain many unanswered questions including how tumors become resistant to daratumumab and if the drug will be active in multiple phases of treatment. In the meantime though, they wrote that “it is reassuring to know that we have yet one more treatment option that will contribute in an important way to improvement in outcomes in patients with myeloma.”