Mutation Status in GIST Has Little Effect on Imatinib Treatment Outcomes
Pathologic and molecular features of gastrointestinal stromal tumors (GIST) were generally not correlated with outcome in a study involving adjuvant imatinib therapy following resection of the primary tumor.
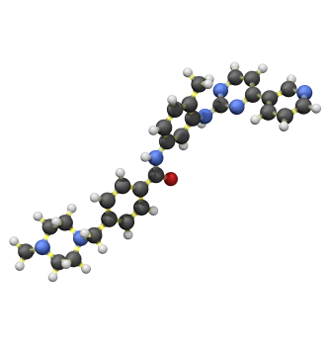
Ball-and-stick model of imatinib
Pathologic and molecular features of gastrointestinal stromal tumors (GIST) were generally not correlated with outcome in a study involving adjuvant imatinib therapy following resection of the primary tumor.
The ACOSOG Z9001 trial found that imatinib prolonged recurrence-free survival after resection vs placebo; researchers led by Christopher L. Corless, MD, PhD, of Oregon Health and Science University in Portland, analyzed 645 tumor specimens from the study to determine pathologic and molecular factors that were associated with outcomes. The results were published online ahead of print in the Journal of Clinical Oncology.
In the original study, 328 patients received placebo and 317 received adjuvant imatinib, and they were followed for a median of 74 months. That study’s main finding, that imatinib improved recurrence-free survival over placebo, was confirmed at longer follow-up in the present analysis. The imatinib patients had a hazard ratio for recurrence of 0.6 (95% CI, 0.43-0.75; P < .001) compared with placebo.
On multivariable analysis, larger tumor size, location of the tumor in the small intestine (vs stomach, rectum, or other), and mitotic rate were all significantly associated with an increased risk of recurrence, in both the placebo and imatinib groups. In the imatinib group, mitotic rate had the largest effect, as those with a mitotic rate of at least 10 per 11.87 mm2 had an HR for recurrence of 4.97. Notably, though, tumor genotype was not significantly associated with recurrence-free survival (P = .13).
“I thought that the impact of genotype on the natural history of GIST… would be bigger than it was,” said Corless in an e-mail. He noted that KIT exon 11 deletions were a factor, while others including those of exon 9 were not-“which contradicts a number of earlier papers.” The study showed that patients with a KIT exon 11 deletion of any type was associated with higher recurrence-free survival in imatinib patients compared with placebo patients, but KIT exon 11 insertions or point mutations, KIT exon 9 mutations, PDGFRA mutations, or wild-type tumors showed no difference between the two treatment groups.
In an accompanying case study in the same journal, William D. Tap, MD, and Gary K. Schwartz, MD, of Memorial Sloan-Kettering Cancer Center in New York, wrote that the study confirms the importance of “tumor size, location, and mitotic rate and indicates that except possibly for patients with KIT exon 11 mutations characterized by deletions, mutational status does not alter the risk recurrence profile for patients with resected primary GISTs.”