NCI Urges Support of Ongoing Breast Cancer Transplant Trial
BETHESDA, Md-Despite bad press and negative scientific findings to date, the National Cancer Institute has not written off high-dose chemotherapy with bone marrow or stem cell transplant as a treatment for breast cancer. Indeed, NCI director Richard D. Klausner, MD, has publicly appealed to oncologists to support a major ongoing but faltering NCI-sponsored breast cancer transplant trial.
BETHESDA, MdDespite bad press and negative scientific findings to date, the National Cancer Institute has not written off high-dose chemotherapy with bone marrow or stem cell transplant as a treatment for breast cancer. Indeed, NCI director Richard D. Klausner, MD, has publicly appealed to oncologists to support a major ongoing but faltering NCI-sponsored breast cancer transplant trial.
The largest trial testing this question [of the therapys effectiveness] is still open, but is in dire need of your support, Dr. Klausner wrote in a letter to members of the American Society of Clinical Oncology (ASCO). The trial needs 1,000 patients and so far has accrued just over 500. If accrual does not pick up, then results from this trial, originally anticipated in 2002, will not be available for many more years.
The NCI director noted that in spite of discouraging preliminary findings from several studiesresults that have adversely affected enrollment in NCIs trial S9623the rationale behind the treatment approach remains sound.
He added that S9623 tests the effectiveness of transplant in a different subset of patients than those treated in previous NCI-sponsored studies and that the negative results from those trials may not apply to patients in the current study.
Better therapies are desperately needed for women at high risk of recurrence, Dr. Klausner said. Whether or not high-dose chemotherapy is a useful therapy for such women can only be determined if clinical trials testing this question appropriately are successfully completed.
S9623 is being led by SWOG (the Southwest Oncology Group), with Scott Bearman, MD, of the University of Colorado Health Sciences Center, as the principal investigator. It targets women with four or more positive lymph nodes who are at high risk of breast cancer recurrence. Participants are randomized to either a high-dose chemotherapy/transplant group or one that receives G-CSF (Neupogen) to support high-dose chemotherapy without transplantation.
Results from this trial will have important implications for both patients and physicians, Dr. Klausner said.
NCI began sponsoring a series of phase III high-dose chemotherapy/transplant trials in 1990 after phase II trials showed promising complete response rates among women with advanced disease. However, its potential as a breast cancer treatment has been heatedly debated over the last decade, and particularly since several US and European teams reported at the 1999 ASCO meeting (Atlanta) that their preliminary results failed to show the treatment was superior to standard therapy.
The only trial reported at the meeting to show a significant advantage for transplanta study reported by Werner Bezwoda, MD, PhD, of the University of Witwatersrand, Johannesburgwas later found to contain fraudulent data.
Emotions regarding transplant continue to run high, Dr. Klausner said in his letter. The question has been hotly debated in courtrooms, in legislatures, and especially in the media. Sentiment among patients and physicians shifts rapidly as each piece of new data becomes available.
He warned not to equate appropriate condemnation of the South African trial with condemnation of transplant. While there are experts who feel existing data suggest that ongoing trials will be negative, others are more optimistic, he said. The only way to resolve this disagreement is through participation in large, carefully monitored clinical trials.
In a press release issued about Dr. Klausners letter, the NCI noted that leading oncologists outside the institute have urged the continuation of transplant studies in breast cancer. It cited, as an example, an editorial in Cancer Investigation in which Dr. Bearman wrote that many more trials will be required before a consensus about the value of dose intensity for breast cancer emerges.
Many patient advocacy organizations have taken similar positions. It would be shortsighted to close the door on all transplant trials for breast cancer based on the information we have right now, said Susan Braun, president of The Susan G. Komen Breast Cancer Foundation.
This is the largest US trial looking at transplant in women with less advanced disease, said Jeff Abrams, MD, who coordinates breast cancer trials for the NCIs Cancer Therapy Evaluation Program. The hypothesis that a transplant may benefit certain groups of patients is still very much an open question. One of the best shots at improved treatment for certain stages of breast cancer is to complete this trial.
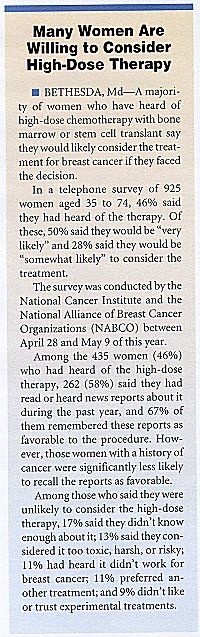
The press release also noted that despite the controversy, a survey indicates that most women would be willing to consider the therapy and to enroll in a clinical trial.