Nedaplatin Improves on Cisplatin in Advanced Lung SCC
The platinum compound nedaplatin in combination with docetaxel improved outcomes over cisplatin and docetaxel in advanced squamous cell carcinoma of the lung.
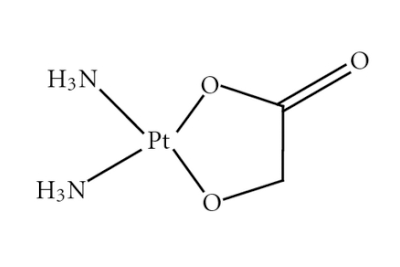
Chemical structure of nedaplatin
The second-generation platinum compound nedaplatin in combination with docetaxel improved outcomes over cisplatin and docetaxel in a phase III trial of advanced squamous cell carcinoma (SCC) of the lung (abstract 8004). Results were presented at the 2015 American Society of Clinical Oncology (ASCO) Annual Meeting, held May 29 to June 2, in Chicago.
“Squamous cell histology accounts for 20% to 30% of non–small-cell lung cancer [NSCLC],” said Takehito Shukuya, MD, of Juntendo University in Japan. “Limited progress has been made in treatment for advanced [lung SCC] when compared to non-squamous NSCLC.” Nedaplatin has shown promising activity in lung SCC in previous phase II trials, and has lower nausea/vomiting and nephrotoxicity rates than cisplatin.
In the new trial, 355 chemotherapy-naive patients with stage IIIb/IV/recurrent disease were randomized to either nedaplatin and docetaxel (ND; 178 patients) or cisplatin and docetaxel (CD; 177 patients); of those, 177 and 172 were evaluable for efficacy.
The study met its primary endpoint: the median overall survival with ND was 13.6 months, compared with 11.4 months with CD, for a hazard ratio (HR) of 0.81 (90% CI, 0.67–0.98; P = .037). The 1-year overall survival rates were 55.9% with ND and 43.5% with CD; at 2 years, the overall survival rates were 27.1% with ND and 18.1% with CD.
The median progression-free survival was 4.9 months with nedaplatin and 4.5 months in the CD group, for an HR of 0.83 (90% CI, 0.69–1.00; P = .050). The 6-month progression-free survival rates in the two groups were 35.6% and 27.9%.
There were no significant differences with regard to response rates, at 55.8% with ND and 53% with CD (P = .663). Subgroup analyses showed better survival outcomes in those with a performance status of 1 and in stage IV disease. In the ND group, 78% went on to second-line therapy and 53.7% went on the third-line therapy; in the CD group, these rates were 76.7% and 40.1%.
All patients in the study experienced some toxicity; grade 3 or higher events were seen in 91.5% of ND patients and in 89.7% of CD patients. Adverse events leading to discontinuation occurred in 15.3% and 23.3% of patients, respectively.
“Nedaplatin plus docetaxel will be considered as a new standard treatment for advanced or relapsed [lung SCC],” Shukuya concluded.
The discussant for the session, David R. Gandara, MD, of the UC Davis Comprehensive Cancer Center, said that conclusion is only partially correct. The study used a dose of docetaxel that is approved in Japan but not in the United States or other countries. “Reproducing the study in a western population would be required before global adoption,” Gandara said.