Neoadjuvant Weekly Paclitaxel Ups Breast Cancer Pathologic Complete Response Rates
SAN FRANCISCO-Preliminary results of an ongoing phase III study suggest that weekly paclitaxel (Taxol) followed by FAC (fluorouracil/Adriamycin/cyclophosphamide) provides improved pathologic complete response rates, compared with standard paclitaxel followed by FAC, M.D. Anderson researchers reported at the 37th Annual Meeting of the American Society of Clinical Oncology (ASCO), held in San Francisco.
SAN FRANCISCOPreliminary results of an ongoing phase III study suggest that weekly paclitaxel (Taxol) followed by FAC (fluorouracil/Adriamycin/cyclophosphamide) provides improved pathologic complete response rates, compared with standard paclitaxel followed by FAC, M.D. Anderson researchers reported at the 37th Annual Meeting of the American Society of Clinical Oncology (ASCO), held in San Francisco.
Marjorie Green, MD, a fellow in Medical Oncology, and her colleagues received the ASCO Merit Award 2001 for this poster presentation.
Patients who achieve a pathologic complete response after neoadjuvant chemotherapy have superior survival, compared with similarly staged patients who have persistent disease following neoadjuvant therapy.
In this ongoing trial, patients were randomized to receive either weekly paclitaxel or paclitaxel every 3 weeks to determine if different schedules or dose densities of this agent improve pathologic complete remission.
"Weekly Taxol has been evaluated widely in the metastatic setting, and it is known to be better tolerated," Dr. Green said. "The question is whether it gives the same response and whether schedule dependence really makes a difference. Preclinical studies suggest that it does."
A previous phase II study by Akerly using weekly paclitaxel 175 mg/m2 "achieved an incredible 86% response," she said. "If we can do this in the adjuvant and neoadjuvant settings, maybe there will be a survival difference."
The dose of weekly paclitaxel in this study was determined by the patient’s pretreatment nodal status. Patients with node-negative disease received 80 mg/m2 a week for 12 weeks and those with node-positive disease received 150 mg/m2 a week for 3 weeks followed by a 1-week break for a total of four cycles.
Patients receiving standard paclitaxel (both node positive and node negative) received paclitaxel 225 mg/m2 as a 24-hour infusion every 3 weeks for four cycles. (This dose was modified to reduce toxicity, and most patients actually received 150 mg/m2.) All patients received four cycles of FAC after completion of paclitaxel, and then local therapy. Node-positive status was confirmed by fine-needle aspiration biopsy.
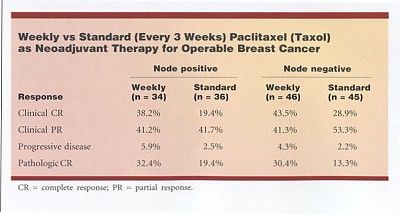
Of 70 node-positive patients, 68 were evaluable; of 91 node-negative patients, 89 were evaluable. Among the 157 evaluable patients to date, the overall pathologic complete response was significantly improved by the weekly schedule vs the standard schedule, approximately 30% vs 15% (see Table), Dr. Green reported.
"This is very encouraging," she said. "We think it’s the weekly regimen that is making a difference. If it were just the volume of disease, you would expect that there would be a lower percentage of patients who had a pathologic complete response with our standard regimen. We think it is the schedule as opposed to the dose."
This ongoing study will accrue 485 patients, about half of whom will undergo neoadjuvant therapy (preliminary results reported here) and half adjuvant therapy. The primary endpoint will be survival.