With New Melanoma Drug, Clinical Trials System Shows Its Age
Patients with advanced melanoma now have access to the BRAF inhibitor PLX4032, which has shown survival advantages in a Phase III trial, as long as they have the "right" mutation. The drug's history so far is proving a case study on the challenges of developing personalized cancer treatment.
How many patients have pleaded with you to help them get the latest drug against advanced melanoma? Mercifully, those whose melanoma cells are vulnerable to the BRAF inhibitor PLX4032 now have access to the drug, either as "crossover" cases in the control arm of the randomized trial that showed its power or as beneficiaries of an Expanded Access Program.
The drug has shown a long-awaited survival benefit. In recently announced that in a multicenter Phase III trial, PLX4032 (which co-developed Roche calls RG7204, but the name hasn't stuck yet) produced significantly longer overall survival among previously untreated patients compared to the treatment standard, dacarbazine. (The companies have not yet released the actual data, but promise to do so at a meeting later this year.)
This result was expected and hoped for: The older drug slows tumor growth in only about 15% of patients for two months, according to historical data. In contrast, PLX4032 slowed it by 81% for eight months in a Phase 1 trial.
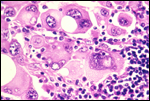
“For the first time, a personalized investigational medicine, RG7204, has shown a significant survival benefit in metastatic melanoma," said Roche CMO Hal Barron, MD. It's "personalized" in that the drug works for only patients whose tumors have the single-nucleotide V600E mutation in BRAF that confers malignant tranformation. Some 60% of melanomas do.
The Expanded Access Program now makes the drug available to previously untreated melanoma patients not enrolled in the trial whose tumors have the V600E mutation. If and when the drug is approved, Roche plans to market a test for the mutation alongside it, so that doctors can determine quickly which melanoma patients should receive it.
Unethical botched protocol?
"Let's hope this common sense approach will propagate into other trials, and humans will no longer be treated on the same level as laboratory mice," wrote a contributor to a melanoma patients' online forum in response to the announcement of the Phase III trial results. "The unethical botched protocol for this trial may have been a blessing in disguise as it really highlighted the need for changes."
But was it really "botched" and unethical? Could we have known that the BRAF inhibitor actually improved survival outcomes without the Phase III trial?
Late-stage melanoma patients were clamoring for PLX4032 long before it was featured in a four-part series in the New York Times last year. One article in the series featured a pair of first cousins with melanoma, both enrolled in the Phase III trial, one of whom was randomized to receive PLX4032 and the other of whom was not. (Guess which cousin is still alive.)
More recently, an editorial the New England Journal of Medicinechose PLX4032 Phase III trial as a case study in examining the problems with "equipoise," the philosophy that allows doctors to deny patients access to a drug not yet proven lifesaving in a randomized trial. Equipoise would hold that, however dramatic a drug's outcomes in terms of surrogate endpoints like tumor shrinkage, doctors can morally enroll patients in randomized trials if there is "professional uncertainty" about its merits.
Calling PLX4032 a "genuinely difficult case,"NIH bioethicist Franklin Miller and Dana-Farber pediatric oncologist Steven Joffe rode the fence in their conclusion. From the perspective of doctors and individual patients, randomized trials of the drug are clearly unethical when the surrogate endpoints are as dramatic as they were for PLX4032, they said. But for policy makers such as the FDA, they added, trials are "both ethical and necessary" to develop evidence for decisions made on behalf of entire populations.
Not a miracle cure
For all the publicity, this is no miracle drug: Tumors inevitably develop resistance to PLX4032 after several months, and researchers have moved quickly to learn why. Unlike other tumors that have found ways to evade kinase inhibitors, melanomas apparently don't develop different mutations in BRAF in response. They appear to resort to other kinase molecules to reach the same end in the MAP biochemical pathway, or to upregulate other growth-receptor pathways to compensate.
Using PLX4032 in combination with other targeted inhibitors is the obvious strategic response to this resistance. A phase I trial is already underway, matching the BRAF inhibitor an inhibitor of the MEK pathway, which is downstream from BRAF on the route to malignant transformation. Very likely more alternative pathways will be discovered, and different inhibitors will be required, mandating further trials of efficacy.
As you might expect, alternative BRAF inhibitors are in development that may show activity in tumors other than melanoma. Combining PLX4032 with the other hot new melanoma drug, ipilimumab (an immune stimulator, not a growth-pathway inhibitor) is also under discussion. This is more like aiming two different weapons at the same target than like increasing the accuracy of the strike.
How quickly will more Expanded Access programs be launched, as and when trials with these other drugs or combinations show initial success? When a drug is shown relatively safe and effective in blocking a specific pathway, how will controlled trials continue to attract enough patients to establish survival endpoints against older, accepted treatments?
The answers to these questions are as yet unknowable. What we can know with certainty is that both research and news about it will proceed with extraordinary speed, and that policy changes will continue to take place with great deliberation. As for oncologists, caution is advised on the road to personalized medicine.