New Therapeutic Target, MDM4, Found in Cutaneous Melanoma
A new target of melanoma tumors has been identified that may be promising as part of a novel combination therapy for melanoma. In a study published in Nature Medicine, researchers have identified that more than half of melanoma cases, both early and late-stage, may have higher levels of MDM4, a p53-interacting protein.
A new target of melanoma tumors has been identified and may be promising as part of a novel combination therapy for melanoma. In a study published in Nature Medicine, researchers have identified that more than half of melanoma cases, both early and late stage, may have higher levels of a p53-interacting protein.
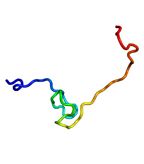
Structure of the MDM4 protein; source: Emw, Wikimedia Commons
While the TP53 gene, which encodes the tumor protein 53, is found mutated in the vast majority of tumors, TP53 is intact in more than 95% of melanomas. The p53 tumor suppressor pathway is important for most cancers, preventing neoplastic growth, and inactivation of the pathway is a common driver mutation for cancer.
Exploring alternative mechanisms of dysregulation of the p53 tumor suppressor pathway, Jean-Christophe Marine, the Center for Human Genetics in Leuven, Belgium, and colleagues show that the pathway is indeed altered in as many as 65% of human melanomas. Rather than a mutation in TP53, the researchers find that melanomas have upregulated Mdm4 p53 binding protein homolog (MDM4), a negative regulator of p53. According to the authors, the results identify “MDM4 as a key determinant of impaired p53 function in human melanoma.”
The preclinical data also suggest melanoma cells resistant to BRAF inhibitors, an approved therapy for metastatic melanoma, can respond to inhibition of the p53 pathway providing a new avenue of combination therapies to explore. Inhibition of MDM4 was also found to sensitize melanoma cells to conventional chemotherapy.
Importantly, targeting the p53 pathway is likely not limited to only BRAF-mutated melanomas, as the study shows MDM4 overexpression occurs equally among both BRAF wild-type and BRAF-mutated melanoma tumors.
The Results
The study shows MDM4 overexpression contributes to more robust cell division and survival in both human cells and in mice. The researchers demonstrate overexpression of MDM4, in addition to an NRAS mutation, results in more tumor development more quickly in a mouse model. The authors find high levels of MDM4 protect melanoma cells from p53-mediated apoptosis.
The study used a peptide, SAH-p53-8, that can disrupt the p53-MDM4 complex by binding to the p53-binding pocket of MDM4 with high affinity. Both cell line and mouse model experiments support the therapeutic potential of honing in on p53 pathway inhibition. All human melanoma cell lines tested were sensitive to MDM4 inhibition, including BRAF-mutated cell lines derived from tumors resistant to BRAF-inhibitors. At least in tissue cultures, the combination of vemurafenib (Zelboraf), and the p53 pathway-targeting peptide were synergistic in decreasing viability of melanoma cells. In a xenograft model, the peptide alone was able to reduce tumor growth.
“Melanomas do not harbor MDM4 mutations per se,” explained Jean-Christophe Marine. “They select for mechanisms that cause MDM4 protein levels to go up.” Marine and colleagues are currently investigating the mechanisms of MDM4 upregulation.
A New Molecular Pathway to Exploit
Approximately 50% of melanoma cases harbor a mutation in the BRAF gene, part of the mitogen-activating protein kinase (MAPK) pathway that results in constitutive activation of the MAPK pathway. A specific inhibitor of BRAF, vemurafenib, was approved last year for metastatic melanoma patients with the BRAF mutation and two other targeted inhibitors of the MAPK pathway, dabrafenib and trametinib, have recently completed phase III trials. While treatment with a BRAF inhibitor results in rapid tumor shrinkage and symptom relief, resistance is still a major issue and new agents and combinations are needed for sustaining prolonged responses.
“The whole field is looking for drugs that can prevent relapse,” said Marine. “Awakening the p53 pathway in melanoma, by targeting MDM4, could be one way to achieve this-a possibility that has so far been completely overlooked.” The p53 pathway has been majorly overlooked in melanoma because the mechanism by which p53 is inactivated in this tumor were unknown until this study.
The current research suggests targeting the important p53 tumor suppressor pathway in melanoma has potential for both BRAF mutated and BRAF wild-type versions of the cancer. The authors highlight previous efforts to target this pathway via MDM2 inhibition did not result in great results, as targeting of MDM2 is not enough in cells that also overexpress MDM4. MDM2 is another negative regulator of p53. The current study suggests that an MDM4-targeting approach is promising in melanoma as most melanomas have high MDM4 levels but low MDM2 levels-high MDM2 melanoma tumors are quite rare, according to the authors. There is a possibility that the peptide used in the study not only targets MDM4, but also MDM2.
From Lab to Clinic
Because the immunofluorescence technique used to detect higher MDM4 expression is not easily implemented in the clinic, according to Marine, he and his team are developing an easier diagnostic method to assess MDM2, MDM4, and p53 protein levels from a small clinical tissue sample-as little as a few cells.
“We hope that stapled peptides could be used in the clinic but several companies are also trying to develop MDM4 specific small molecule antagonists,” said Marine. A derivative of the protein nutlin, nutlin-3a, targets MDM2, and is currently in clinical trials.
“Importantly while there is data indicating that MDM2 antagonist might be toxic to patients we and others have provided evidence indicating that MDM4 antagonist should be safer-less toxic to patients than MDM2 antagonists,” said Marine.