New Therapeutic Targets for Small-Cell Lung Cancer Identified
For the first time, two research groups have sequenced and analyzed the genomes of small-cell lung cancer (SCLC) and identified new gene mutatations that could drive the development of new therapies and the application of existing ones.
For the first time, two research groups have sequenced and analyzed the genomes of small-cell lung cancer (SCLC), identifying new gene mutations that could drive the development of new therapies as well as the application of existing therapies to this difficult-to-treat cancer type. This type of analysis is particularly important, as there are currently no molecularly targeted drugs for SCLC.
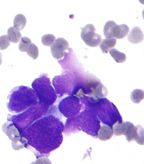
Micrograph of small-cell carcinoma of the lung; FNA specimen; field stain; source: Nephron, Wikimedia Commons
The two studies, published in Nature Genetics, sequenced a total of 82 SCLC tumor samples. Because SCLC is rarely treated with surgery, tumor samples are rare, making the analysis of a large number of tumors difficult.
“The two reports provide us with a new framework from which to initiate future drug development in [SCLC], highlighting that SCLC samples can be collected and analyzed using next generation sequencing and comprehensive genomic profiling,” said M. Catherine Pietanza, MD, lung cancer oncologist at Memorial Sloan-Kettering Cancer Center in New York. “In-depth genomic sequencing studies such as these are extremely useful in lung cancer, and in oncology in general.”
Lung cancer is still the leading cause of cancer deaths in the United States, accounting for about 160,000 deaths every year. SCLC accounts for about 15% of all lung cancer cases.
SCLC is histologically distinct from non–small-cell lung cancer (NSCLC). SCLC typically has a high nuclear to cytoplasmic ratio, a high mitotic index, and neuroendocrine markers, according to Ross Camidge, MD PhD, director of the thoracic oncology clinical program at the University of Colorado Cancer Center in Aurora, Colorado. The cancer type is more aggressive compared to NSCLC, grows quickly, and metastasizes early compared to other cancer types. While patients with SCLC initially have a high response to chemotherapy, relapse and resistance to treatment is quite rapid. SCLC occurs predominantly in heavy smokers.
SCLC, even at earlier stages, has a low cure rate and unlike with NSCLC, resection is rare. Early stage SCLC is typically treated with a combination of chemotherapy and radiotherapy to all involved sites, according Camidge. The goal is to attempt to cure the disease. Unfortunately, SCLC is typically diagnosed at a later stage of the disease and therefore difficult to treat. Frontline treatment for late-stage disease is platinum-based chemotherapy, cisplatin or carboplatin, along with etoposide. “Although numerous other chemotherapeutic regimens have been evaluated, this doublet has been the treatment of choice since its initial evaluation in the late 1970s, predominantly due to the ability to add radiation therapy for those patients with limited-stage disease,” said Pietanza.
Initially, SCLC is responsive to chemotherapy, but most patients recur or progress in weeks to months according to Pietanza. The only approved second-line treatment in both the United States and Europe is topotecan. Patients may also respond to a rechallenge with the same platinum-based therapy, but the duration of response is typically diminished. “No new developments have happened in SCLC in years,” said Camidge. “There have been no targeted agents licensed specific to SCLC.”
Sequencing Studies Results
Roman Thomas of the University of Cologne in Germany and colleagues sequenced 29 SCLC exomes. In a separate study Somasekar Seshagiri, a researcher at Genentech in San Francisco, California, Charles Rudin, MD, PhD, of Johns Hopkins University in Baltimore, Maryland, and colleagues sequenced the exomes of 36 primary SCLC tumors and 17 SCLC cell lines derived from SCLC tumors. The study identified 22 mutated genes and an amplification of the SOX2 gene in more than a quarter of samples, suggesting that SOX2 has an important role as a driver of tumorigenesis in SCLC.
“Small-cell lung cancer is an exceptionally aggressive disease, for which novel therapeutic options are critically needed,” said Rudin. “We hope that defining the genomic landscape of small-cell lung cancer will ultimately lead to new treatment options for patients with this disease.”
The pattern of mutations observed among the SCLC genomes are consistent with the effects of exposure of the DNA in cells to the carcinogens found in tobacco smoke.
“These two new studies and existing prior studies all confirm the enormous number of sequence changing mutations present in each SCLC,” said Camidge. Approximately 175 protein-altering mutations per tumor were found, with one tumor having 757 separate protein-altering mutations.
“Not surprisingly, just as adenocarcinoma of the lung appears to be multiple different diseases when looked at from the perspective of dominant oncogenic driver mutations, SCLC is really multiple different diseases,” said Camidge. Camidge highlighted the remarkably small amount of mutation overlap between the two published studies. The highly varied genomes of SCLC pose a challenge. “Not only do we need to explore whether pharmacological manipulation of some of these novel changes is possible, we also need to see whether it is worthwhile medically,” explained Camidge. Another challenge is that gathering patients for such trials would likely be difficult-patient populations with molecularly defined SCLC subtypes are very small.
Previous studies have identified inactivating mutations in genes mutated in a spectrum of cancer-PTEN, TP53, and activating mutations in the PIK3CA, EGFR, and KRAS genes. In the Rudin et al study, TP53, RB1, PIK3CA, CDKN2A and PTEN were validated as known frequently mutated genes. Among the 22 most frequently mutated genes, the novel genes included Ras family regulators, chromatin-modifying enzymes, and transcriptional regulators. Unlike NSCLC tumor genomes, the researchers did not find any mutations in the KRAS gene. “Currently, there are numerous inhibitors targeting alterations in PIK3CA/PTEN and FGFR1 being evaluated in phase I and II clinical trials that could benefit SCLC patients whose tumors bear these alterations,” said Pietanza.
SOX2, found amplified in SCLC, is a transcription factor necessary for maintaining self-renewal and pluripotency of undifferentiated embryonic stem cells. SOX2 amplification correlated with higher expression of SOX2 in SCLC tumor cells. While SOX2 has been previously implicated in other cancers including squamous-cell lung cancer, there are currently no drugs in development that inhibit SOX2 or other transcriptional factors that bind directly to DNA.
A fusion between RLF and MYCL1, two genes located on the same chromosome, was also identified. The primary tumor from which the fusion was derived overexpressed the MYCL1 gene, a transcription factor previously associated with lung cancer.
The second study by Thomas and colleagues provide evidence for PTEN mutations and fibroblast growth factor receptor 1 (FGFR1) amplifications as being potential therapeutic targets. PTEN was mutated in 3 of the 29 tumors sequenced, all affecting the function of the phosphatase domain of the protein. The authors found a very high mutation rate of 7.4 ± 1 protein-changing mutations per million base pairs. The team found “histone modification as a major feature of SCLC.” TP53 and RB1 were consistently inactivated among the analyzed tumors and were early mutation events. Genes that encode histone-modifying proteins such as CREBBP, EP300, and MLL, were also frequently mutated.
“There are multiple potentially drug-able targets [identified in our study], but validation of these targets needs to be performed to really determine which are relevant in moving the treatment of small-cell lung cancer patients forward,” said Rudin. The authors are actively following up on the initial sequencing results with more in-depth analysis of the pathways that drive SCLC. “This is clearly a major goal, and is an area of active research primed by these data,” said Rudin.
What is the ultimate utility of these types of sequencing analyses? Camidge sees sequencing studies as a way to break down disparately pooled diseases, such as SCLC or triple-negative breast cancer. Embracing heterogeneity and identifying new patterns to generate new hypotheses to test is the best way forward according to Camidge. “As sequencing techniques get cheaper and easier to apply, what seems like out-of-reach science will get to the bedside pretty quickly in years to come,” said Camidge.
“We need to do [sequencing analyses] in a prospective fashion and obtain larger amounts of tissue at the time of initial biopsy for molecular analyses,” said Pietanza. “In addition, collecting tissue at the time of recurrence to perform next generation sequencing may give us more information regarding the biology of the disease and provide insight as to how this disease recurs.”