No Major Racial Disparities Reported in Allogeneic Transplant Outcomes
Study authors note that access to multidisciplinary teams and transportation programs may help mitigate hematopoietic cell transplantation outcome disparities.
“Strategies currently implemented at our institution mitigating HCT outcome disparities could include [reduced-intensity conditioning], [posttransplant cyclophosphamide], letermovir prophylaxis, access to multidisciplinary teams, transportation programs, supported care facilities [posttransplant], and shared care with local facilities easing transportation burden,” according to the study authors.
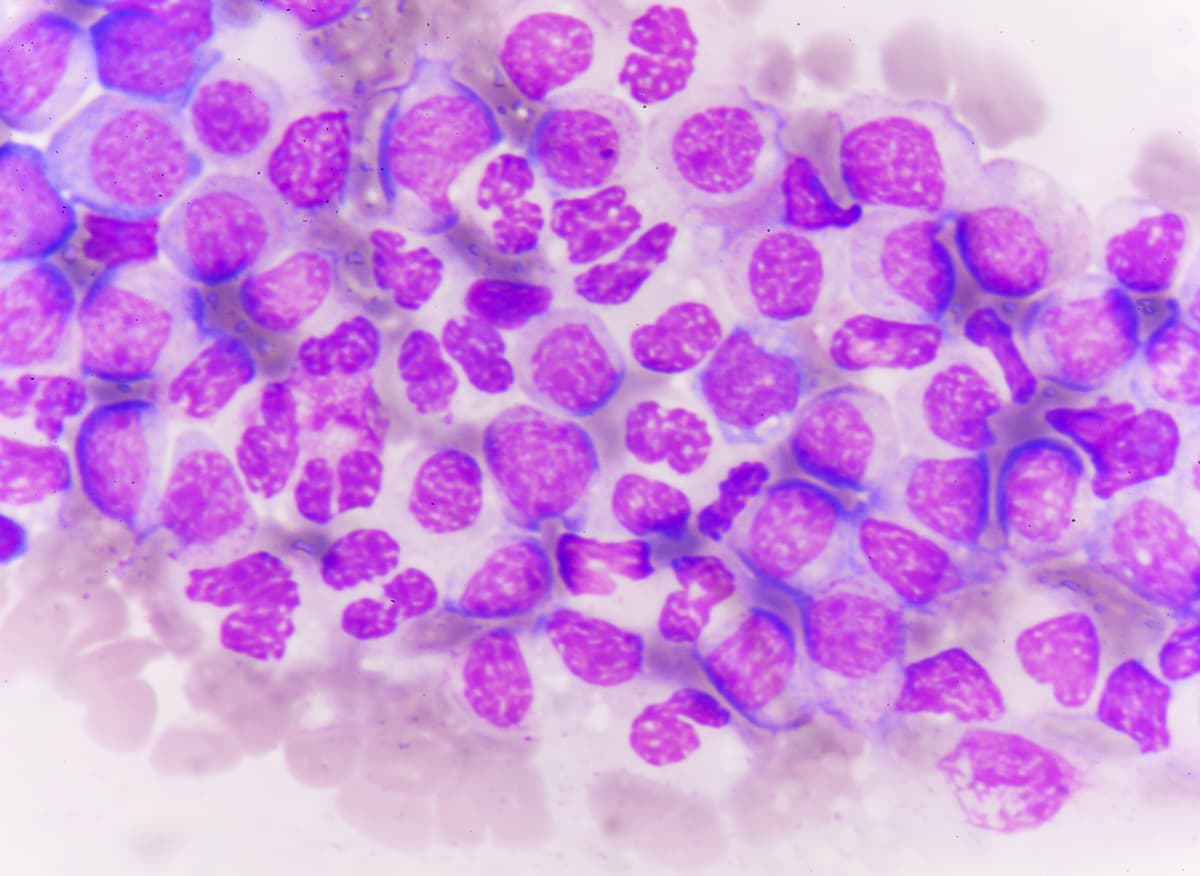
There were no significant racial differences in major outcomes for patients undergoing allogeneic hematopoietic cell transplantation (HCT), although cytomegalovirus (CMV) and Epstein Barr virus (EBV) reactivation tended to occur more frequently in Asian and Black patients, respectively, according to retrospective data that were presented at the 2024 Transplantation and Cellular Therapy Meetings.
Results showed that the 2-year overall survival (OS) rate was similar across ethnic groups, including patients who are East Asian (70.3%; 95% CI, 60.1%-78.3%), Black (66.8%; 95% CI, 50.4%-78.9%), South Asian (66.1%; 95% CI, 53.4%-76.1%), White (65.0%; 95% CI, 60.1%-69.5%), and other races (63.1%; 95% CI, 49.7%-73.8%; P = .96).
Two-year nonrelapse mortality (NRM) rates were 14.3% (95% CI, 8.2%-22.0%) in East Asian patients, 25.9% (95% CI, 13.8%-39.8%) in Black patients, 18.8% (95% CI, 10.6%-28.9%) in South Asian patients, 19.1% (95% CI, 15.4%-23.0%) in White patients, and 17.2% (95% CI, 9.1%-27.5%) in patients of other races (P = .56).
The 2-year cumulative incidence of relapse (CIR) rates were 25.3% (95% CI, 16.8%-34.7%), 16.3% (95% CI, 6.5%-30.1%), 22.4% (95% CI, 12.9%-33.6%), 23.4% (95% CI, 19.3%-27.7%), and 23.1% (95% CI, 13.3%-34.4%) in patients who are East Asian, Black, South Asian, White, and other races, respectively (P = .59).
However, CMV reactivation rates were notably higher in East Asian patients (61.0%; 95% CI, 50.6%-69.8%), South Asian patients (54.3%; 95% CI, 41.8%-65.2%), and Black patients (51.2%; 95% CI, 35.2%-65.1%) compared with White patients (38.3%; 95% CI, 33.7%-42.9%) and patients of other races (46.9%; 95% CI, 34.2%-58.6%; P <.001). A multivariable cox regression analysis confirmed an increased risk of CMV reactivation in East Asian patients (HR, 1.8; P = .0002).
Similar trends were reported for EBV reactivation at 70.0% (95% CI, 59.9%-78.0%), 74.4% (95% CI, 57.9%-85.2%), and 71.4% (95% CI, 59.1%-80.7%) in the East Asian, Black, and South Asian subgroups, respectively, compared with 65.2% (95% CI, 60.5%-69.5%) and 64.1% (95% CI, 50.8%-74.6%) in patients who are White and of other races, respectively (P = .73). A multivariable cox regression analysis confirmed a higher risk of EBV reactivation for Black patients (HR, 1.5; P = .03).
“Strategies currently implemented at our institution mitigating HCT outcome disparities could include [reduced-intensity conditioning], [posttransplant cyclophosphamide], letermovir prophylaxis, access to multidisciplinary teams, transportation programs, supported care facilities [posttransplant], and shared care with local facilities easing transportation burden,” lead study author Elizabeth Herrity, DNP, of the Hans Messner Allogeneic BMT Program at Princess Margaret Cancer Center, University Health Network in Toronto, Ontario, Canada, and coinvestigators wrote in the poster that was presented at the meeting.
Previously, disparities in the access and use of HCT, as well as HCT intervals, have been reported, including diagnosis to HCT intervals. Furthermore, there are little data on whether disparities exist in HCT outcomes or access in Canada for various racial or ethnic groups. In the retrospective review, investigators sought to identify whether these disparities exist by assessing 709 patients of self-identified races and ethnicities undergoing HCT at Princess Margaret Hospital between January 2018 and April 2022.
The coprimary end points were OS, CIR, and NRM. Secondary outcome measures were relapse-free survival (RFS), graft vs host disease (GVHD)-free RFS (GRFS), incidence of acute and chronic GVHD, and CMV and EBV incidence.
Patient race and ethnicity data were self-reported, which reflected congruent studies, geographical birth locations, and population data categories on Canada.ca, specific to Toronto City statistics.
Of the 709-patient population, most were White (n = 432), followed by East Asian (n = 100), South Asian (n = 70), other races (n = 64), and Black (n = 43). The median age was 58 years (range, 18-76; P <.001), and 43.6% of patients were female (P = .85). Additionally, 59.4% of patients had acute leukemia compared with other myeloid malignancies (28.9%) and other diseases (11.7%). A total of 29.2% of patients had HLA-mismatch donors (P <.001). Reduced-intensity conditioning was given in 68.3% of all patients (P = .10), and T-cell depletion was given in 97.6% (P = .02). A total of 35.9% of patients had an HCT-CI score of 3 or greater (P <.001), and 15.5% of patients were CMV serostatus donor and recipient negative (P <.001).
Additional data showed that the 2-year RFS rate was 59.5% (95% CI, 48.6%-68.6%), 53.5% (95% CI, 36.2%-68.1%), 57.9% (95% CI, 44.6%-69.0%), 57.8% (95% CI, 52.8%-62.5%), and 59.1% (95% CI, 45.7%-70.3%) for patients who are East Asian, Black, South Asian, White, and other races, respectively (P = .97).
Further findings showed that the 2-year GRFS rate was similar across the East Asian (49.1%; 95% CI, 38.8%-58.7%), Black (36.6%; 95% CI, 22.4%-50.9%), South Asian (42.8%; 95% CI, 30.8%-54.3%), White (43.7%; 95% CI, 38.8%-48.5%), and other (38.2%; 95% CI, 26.3%-50.1%) racial groups (P = .69).
When evaluating donor source by ethnicity, it was noted that more Black patients had haploidentical donors and more White patients received matched unrelated donors compared with other donor types.
The authors noted that, on a bivariate analysis, Black patients were younger than other patient subgroups by 10 years and were 20% more likely to have an HLA-MM donor and twice as likely to have an HCT-CI score of at least 3.
Reference
Herrity E, Singhabahu S, Remberger M, et al. Exploring outcomes by ethnicity in allogeneic hematopoietic cell transplantation. Transplant Cell Ther. 2024;30(2):S325. doi:10.1016/j.jtct.2023.12.450