Nodal Metastases Linked With Decreased Survival Even in Younger Thyroid Cancer Patients
The presence of cervical lymph node metastases was associated with compromised survival even in younger patients with papillary thyroid cancer.
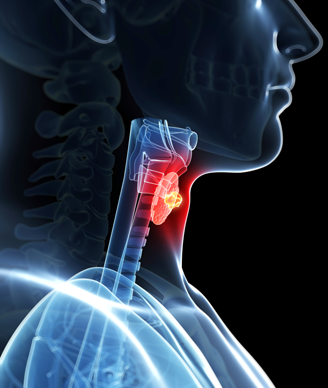
Image © Sebastian Kaulitzki / Shutterstock.com
The presence of cervical lymph node metastases was associated with compromised survival even in younger patients with papillary thyroid cancer, according to results of a new study. This could yield changes to staging guidelines for this disease.
“In the current American Joint Committee on Cancer (AJCC) staging, patients younger than age 45 years with differentiated thyroid cancer are considered to have only two possible stages of disease based on absence (stage I) or presence (stage II) of distant metastases,” wrote study authors led by Julie A. Sosa, MD, of Duke University Medical Center in Durham. As a result, patients with cervical lymph node metastases are considered to have stage I disease.
The role of those lymph node metastases in younger patients has not been well defined, though in older patients their prognostic significance has been established. The new study used National Cancer Data Base (NCDB) and SEER databases to examine the impact of lymph node metastases in younger papillary thyroid cancer patients. Results were published online ahead of print in the Journal of Clinical Oncology.
The study included 47,902 patients in the NCDB (11,740 had nodal metastases and 36,162 did not), and another 21,855 (5,188 with and 16,667 without) patients in the SEER database. The primary analysis showed that overall survival was worse in those with nodal metastases in both cohorts.
In the NCDB cohort, the adjusted overall survival at 5 years was 99.3% for those without nodal metastases, and 99% among those with nodal metastases. This yielded a hazard ratio (HR) of 1.32 (95% CI, 1.04–1.67; P = .21). At 10 years, the survival rates were 98.2% and 97.8%, respectively. The authors also found a significant association between the risk of death and the number of metastatic lymph nodes (P = .046).
In the SEER cohort, results were similar, with an HR for overall survival of 1.29 (95% CI, 1.08–1.56; P = .005). Survival rates were slightly lower for those with nodal metastases compared to those without at 5, 10, 15, and 20 years.
“Although differences in overall survival based on the existence of lymph node metastases were small, it should be noted that they were comparable to those in patients 45 years or older,” the authors wrote, adding that thyroid cancer incidence has increased substantially in recent decades. “With increasing incidence, a small percent change in survival will translate into a significant number of deaths.”
They concluded that the current AJCC staging system may need revision to reflect the importance of nodal metastases.