Novel Treatment Displays Tolerability in Relapsed/Refractory B-Cell ALL
A total of 45% of patients with B-cell acute lymphoblastic leukemia experienced cytokine release syndrome while receiving treatment with MK-1045, of which 3% experienced grade 3 events.
A total of 45% of patients with B-cell acute lymphoblastic leukemia experienced cytokine release syndrome while receiving treatment with MK-1045, of which 3% experienced grade 3 events.
Treatment with MK-1045 in adult patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) displayed a generally manageable safety profile with dose modifications and standard medical care, according to findings from the phase 1b/2 trial (NCT05579132) presented in an oral presentation given at the 2025 American Society of Hematology (ASH) Annual Meeting and Exposition.
Safety data revealed that among 75 patients treated across 9 dose levels on the trial, all had experienced at least 1 treatment-emergent adverse effect (TEAE), 89% of which were grade 3 to 5 in severity. A total of 33% of patients experienced TEAEs leading to dose interruption, and 1% of patients experienced dose reductions or death related to TEAEs. Moreover, no patients experienced dose discontinuations due to TEAEs.
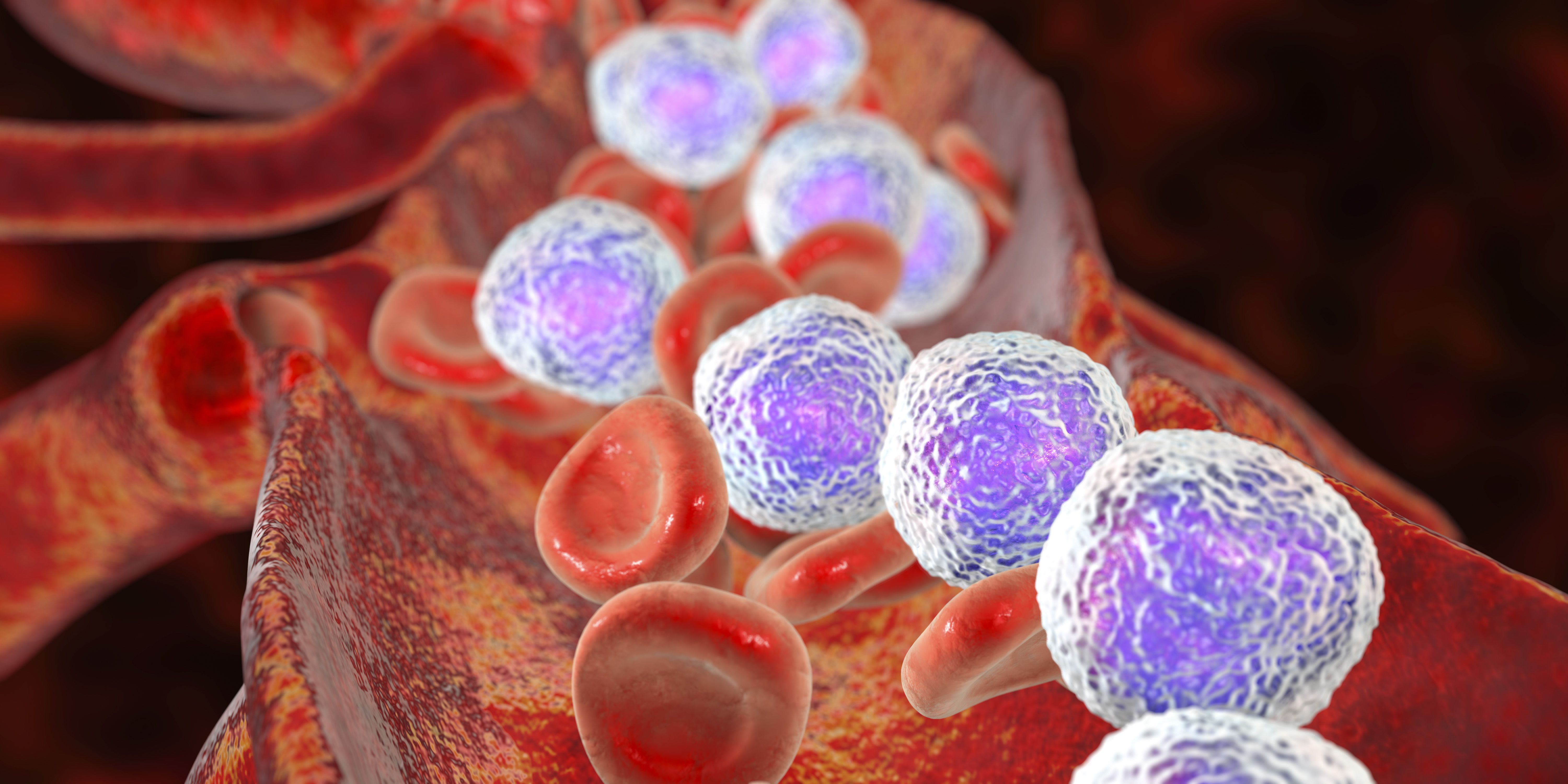
The most common any-grade TEAEs were primarily hematologic and included white blood cell count decreases, neutrophil count decreases, platelet count decreases, lymphocyte count decreases, anemia, and hypokalemia. Similarly, the most common grade 3 or 5 TEAEs were hematologic as well, the most common of which included white blood cell count decreases, lymphocyte count decreases, neutrophil count decreases, platelet count decreases, and anemia.
Regarding the incidence of cytokine release syndrome (CRS), 45% of patients experienced at least 1 event. A total of 43% of events were grade 1 or 2 in severity, with 3% of patients experiencing grade 3 CRS. Notably, no grade 4 or 5 events were observed on the trial.
Moreover, a total of 15% of patients experienced neurotoxicity AEs, of which none were grade 3 to 5 in severity. The most frequent neurotoxicity AEs included headache (8%), dizziness (5%), insomnia (3%), depressed consciousness levels (1%), and peripheral neuropathy (1%). No immune effector cell-associated neurotoxicity syndrome (ICANS) was observed in the trial.
“The safety profile of MK-1045 in adult [patients] with relapsed/refractory B-cell ALL has generally been manageable with dose modifications and standard medical care,” study author Ying Wang, of the Institute of Hematology and Blood Disease Hospital of the Chinese Academy of Medical Sciences and Peking Union Medical College in Tianjin, China, stated in the presentation.“There were no treatment discontinuations due to adverse [effects], CRS occurred in 45% of [patients, and] only 3% were grade 3, and no grade 4 or 5 CRS events occurred. Neurotoxicity occurred in 15% of [patients], all grade 1 and 2; no ICANS occurred.”
Patients in the phase 1b/2 trial had relapsed/refractory B-cell ALL with more than 5% bone marrow blasts, were refractory to primary induction therapy or salvage therapy, experienced a relapse within 12 months following first remission, experienced a second or later relapse, and had an ECOG performance status of 0 to 2. Patients who were Philadelphia chromosome-positive must have received prior treatment with a minimum of 2 tyrosine kinase inhibitors or have T315I mutations.
Treatment in cycle 1 consisted of a priming dose on day 1, an intermediate dose on day 8, and a target dose on day 15 and after of study treatment. Treatment cycles lasted 28 days with 2-week treatment-free intervals, and patients in cycle 2 up to cycle 12 were treated weekly with the target dose of MK-1045. Doses ranged from 0.15, 0.3, and 0.6 mg as priming, intermediate, and target doses, up to 2, 20, and 90 mg, respectively.
Those treated on the study had a median age of 46 years (range, 18-73), and 11% of patients were 65 years and older. A total of 52% of patients were male, and 96% were Han Chinese. Most patients in the study had an ECOG performance status of 1 (69%) and Philadelphia chromosome-negative disease (72%).
The median baseline bone marrow blast percentage was 39% (range, 0%-88%), and most patients had received 1 prior line of therapy (33%). A total of 44% and 39% of patients experienced a relapse within 12 months after the first remission or a relapse to last prior to salvage therapy, respectively. The most common prior therapies included allogenic stem cell transplantation (15%) and CD19xCD3 treatment (11%).
The primary end points of the study were safety and tolerability, dose-limiting toxicities, and establishing the maximum tolerated dose and the recommended phase 2 dose. Secondary end points included complete remission (CR) rate, CR with incomplete hematologic recovery (CRi) or partial hematologic recovery (CRh) rate, and the rate of minimal residual disease (MRD) negativity.
Regarding efficacy data, at the 60 mg and 90 mg (n = 12, 12) dose levels, 75% and 92% experienced a CR as best overall response, with 58% and 75% of patients experiencing a CR with complete hematologic recovery, and 8% of each dose level experiencing a CRi, and 8% of each experiencing a CRh. The MRD-negativity rates were 89% and 91%, respectively. The median duration of CR at each dose level was 11.3 months (IQR, 2.6-not reached [NR]) and NR (range, 2.4-NR).
Disclosures:Wang did not report any relevant disclosures.
Reference
Wang Y, Yin Q, Ren J, et al. Updated results from the phase 1b/2 study of MK-1045, a novel CD19xCD3 T-cell engager, in adult participants with relapsed or refractory B-cell acute lymphoblastic leukemia. Blood. 2025;146(suppl 1):647. doi:10.1182/blood-2025-647