Optimal Strategy in Early Multiple Myeloma: Melphalan, Transplantation, Maintenance
The optimal treatment strategy for newly diagnosed multiple myeloma is consolidation with melphalan, stem-cell transplantation, then lenalidomide maintenance.
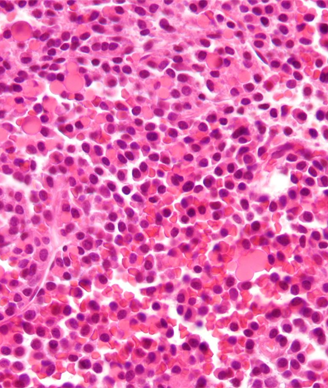
Micrograph of a plasmacytoma; copyright 2009 Nephron.
The optimal treatment strategy for patients with newly diagnosed multiple myeloma is consolidation therapy with high-dose melphalan plus stem-cell transplantation, followed by maintenance therapy with lenalidomide, according to the results of a phase III trial published recently in the New England Journal of Medicine.
“The best treatment strategy was associated with a 5-year rate of progression-free survival from the time of diagnosis of approximately 48% and an overall survival rate of 78% among all patients,” wrote author Antonio Palumbo, MD, of the University of Turin, Italy, and colleagues. “These results confirm a net clinical benefit of high-dose melphalan administration as consolidation treatment and provide support for the benefit of lenalidomide as continuous treatment.”
These treatment strategies were compared to treatment with melphalan-prednisone-lenalidomide (MPR) and the use of no maintenance therapy.
Recent advances in multiple myeloma with orally administered drugs have called into question the role of autologous stem-cell transplantation in the treatment of the disease. In addition, available data are lacking on whether the use of maintenance therapy after combination therapy will have the same effect on outcomes as it does when used after transplantation.
Palumbo and colleagues explored both of these questions in a phase III study that included 273 patients with newly diagnosed multiple myeloma who were randomly assigned to high-dose melphalan (200 mg per m2 of body surface) plus stem-cell transplantation (n = 141) or MPR (n = 132), followed by random assignment to maintenance therapy with lenalidomide or no maintenance therapy.
Looking at the total enrolled population, the median progression-free survival was 54.7 months for high-dose melphalan plus lenalidomide maintenance; 37.4 months for high-dose melphalan with no maintenance therapy; 34.2 months for MPR plus lenalidomide maintenance; and 21.8 months for MPR with no maintenance therapy.
The 5-year overall survival rate was highest in patients who underwent treatment with high-dose melphalan plus stem-cell transplantation and maintenance therapy (78.4%), and lowest in those who received MPR with no maintenance therapy (58.7%).
“At the end of the induction and mobilization phase, the random assignment to high-dose melphalan or MPR was disclosed for the 273 patients who were eligible for consolidation therapy,” the researchers wrote.
Overall, patients who received high-dose melphalan had significantly longer progression-free survival than those who received MPR (43 months vs 22.4 months; P < .001). The 4-year overall survival was also significantly longer in patients who received high-dose melphalan (81.6% vs 65.3%; P = .02). A subgroup analysis showed that the progression-free survival benefit was consistent across all subgroups.
Among the 251 patients who were randomly assigned to maintenance therapy or no maintenance therapy, analyses showed that treatment with lenalidomide results in a significantly longer progression-free survival compared with no maintenance therapy (41.9 months vs 21.6 months; P < .001). However, the 3-year overall survival was not significantly longer with maintenance therapy (88% vs 79.2%; P = .14).
Patients assigned to high-dose melphalan had higher rates of grade 3 or 4 neutropenia, gastrointestinal adverse events, and infections compared with those assigned MPR. Additionally, those patients who underwent maintenance therapy had higher rates of neutropenia and dermatologic toxic effects.
“Ongoing large collaborative studies are evaluating effective drug combinations that include a proteasome inhibitor vs autologous stem-cell transplantation, the benefit of early vs late transplantation, and the effects of varying the duration of maintenance therapy,” the researchers wrote. “Results of these trials may shed further light on this important clinical area.”