Osteoporosis Seen in Patients on Long-Term Androgen Deprivation
ATLANTA-For men with advanced or recurrent prostate cancer, 24 months of androgen deprivation accelerates bone loss, and these changes were significant at sites such as the forearm and hip, David M. Preston, MD (Maj., Medical Corps, U.S. Army), reported at the 95th Annual Meeting of the American Urological Association (AUA).
ATLANTAFor men with advanced or recurrent prostate cancer, 24 months of androgen deprivation accelerates bone loss, and these changes were significant at sites such as the forearm and hip, David M. Preston, MD (Maj., Medical Corps, U.S. Army), reported at the 95th Annual Meeting of the American Urological Association (AUA).
At the same meeting, Yasuyuki Suzuki, MD, Jikei University Hospital, Tokyo, reported that the initial protection provided by adjuvant treatment with vitamin D is not sustained over 12 months, but low doses of estrogen slow bone loss, and use of a statin (HMG-CoA reductase inhibitor) might reverse it.
Prior to the widespread use of serum PSA testing, patients with advanced prostate cancer were treated with androgen deprivation based on symptomatic metastasis or abnormal bone scans, Dr. Preston told ONI. In the PSA era, androgen deprivation is initiated earlier, thus exposing patients to the therapy for longer periods and increasing their risk of significant bone loss. Dr. Preston is in the Department of Urology, Evans U.S. Army Hospital, Ft. Carson, Colorado.
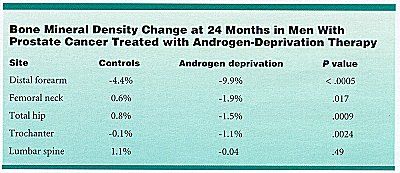
Dr. Preston reported data from a prospective study comparing bone mineral density changes and urine markers of bone degradation in 39 subjects receiving androgen-deprivation therapy and 39 age-matched controls. Subjects were evaluated every 6 months for 24 months. This report included data from the 22 androgen-deprivation subjects and 30 control subjects who completed the 2-year study.
The androgen-deprivation group had greater rates of bone mineral density loss than the control group at every site except the lumbar spine, Dr. Preston said. In addition, urine markers of bone degradation were higher in the androgen-deprivation group than in the controls, although these markers did not change significantly during the study period within groups. The two groups had similar exercise habits, daily dietary calcium intake, and body mass indices.
Dr. Preston said that these findings indicate that men receiving androgen-deprivation therapy are at increased risk of bone-related complications such as osteoporosis and bone fractures.
He recommended baseline and surveillance bone mineral density measurements for all prostate cancer patients undergoing androgen deprivation. Medical therapy to halt or reverse bone loss should be considered in those patients who demonstrate osteoporosis by bone mineral density measurement, Dr. Preston said.
Dr. Suzuki reported pilot observations from prostate cancer patients treated with androgen deprivation who were also given an activated form of vitamin D3 (alfacalcidol, 1 µg/day, n=35); low-dose estrogen (diethylstilbestrol, 100 mg/day, n=14); or standard-dose estrogen (300 to 600 mg/day, n = 11). He also described two patients who coincidentally had been taking a statinpravastatin (Pravachol) or simvastatin (Zocor)for 2 years to treat hyperlipidemia. Bone mineral density changes were compared with data from historical controls.
Bone density loss in men treated with androgen deprivation was about 5% per year. In those treated with either dose of diethylstilbestrol, this dropped to nearly zero. In men treated with vitamin D, the loss dropped to 2.8% (not a significant improvement), and in the two men who were taking a statin, bone density increased by 1.7%.
Dr. Suzuki told ONI that he was surprised at the statin effect. This drug is used safely to treat hyperlipidemia. Now I am using it for patients with prostate carcinoma who are being treated with androgen deprivation. Next year I hope to be able to report the true effect of a statin in these patients, he said.
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.