(P105) Improving Clinical Outcomes in Definitive Treatment of Esophageal Cancer Using a Novel Endoesophageal 3-Tube HDR Technique
To review our local control (LC), survival, and swallowing outcomes using an innovative endoesophageal brachytherapy technique. Further, we conducted a dose-volume comparison for clinical target volume (CTV) using the standard 1-tube vs our novel 3-tube technique.
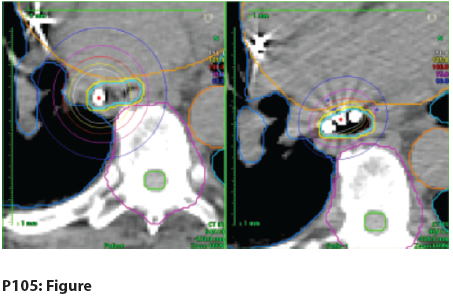
P105: Figure
John F. Greskovich, MD, Matt D. Kolar, MS, Allan Wilkinson, PhD, Andrew Godley, PhD; Cleveland Clinic
Purpose and Objectives: To review our local control (LC), survival, and swallowing outcomes using an innovative endoesophageal brachytherapy technique. Further, we conducted a dose-volume comparison for clinical target volume (CTV) using the standard 1-tube vs our novel 3-tube technique.
Materials and Methods: We retrospectively reviewed the initial 13 medically unresectable, stage 0–IVA esophageal cancer patients treated with endoesophageal high-dose-rate (HDR) brachytherapy using a novel 3-tube technique. Five patients were treated with definitive HDR alone, and eight were treated with definitive combined external beam radiation therapy (EBRT) plus HDR. Two of eight EBRT + HDR patients received concurrent cisplatin/5-fluorouracil (5-FU) at weeks 1 and 4 of EBRT. Kaplan-Meier analysis was used to determine disease-free survival (DFS), overall survival (OS), and LC. The dose-volume relationship for CTV and implant volume for the 1-tube vs 3-tube technique planned with V100 of 90% in our initial patient was completed. Dice’s coefficient (DC) was calculated in 11 patients who underwent 43 total HDR applications and 36 3-tube vs 7 1-tube procedures.
Results: Of 13 medically unresectable patients, 11 were male and 2 were female, with a mean age of 72 years (range: 52–90 yr). Histology was adenocarcinoma in nine patients and squamous cell carcinoma in four patients. Tumor was located in the distal, middle, and proximal one-third of the esophagus in 10 patients, 2 patients, and 1 patient, respectively. Stage 0, 1A, 1B, 2A, 2B, 3A, and 4A occurred in one, one, six, one, one, two, and one of the patients, respectively. The HDR-alone dose was 25–30 Gy (mode 30 Gy) in 5–6 weekly fractions of 5 Gy/fx. The HDR dose after EBRT was 10–25 Gy (mode 15 Gy) in 2–5 weekly fractions. The EBRT dose was 50–64 Gy (mode 50 Gy). Of the five stage 0–1B HDR-alone patients, four are alive without disease (no evidence of disease [NED]); one is alive with distant failure (DF) in the lung/pleura. No local failures (LFs) occurred in five HDR-alone patients. Of the eight stage 1B–4A HDR + EBRT patients, five are alive with NED, one is alive with NED after cryotherapy for LF, and two are dead of distant failure in the liver. One of eight HDR + EBRT patients has LF but was salvaged with cryotherapy. Overall, 2 of 13 patients experienced LF after HDR +/− EBRT. At a median follow-up of 17.4 months, 18-month OS is 92.3%, 18-month DFS is 74%, and 18-month LC is 81%. No fistulas were seen. Two of 13 patients required dilatation for stricture. Eleven of 13 patients denied dysphagia, and 2 of 13 patients had grade 2 dysphagia, one requiring a stent.
The V100, V150, V200, and V300 were 90.0%, 73.5%, 62.3%, and 46.0% vs 90.2%, 66.7%, 41.5%, and 17.7%, for the 1-tube vs 3-tube technique, respectively. For the 3-tube technique, the implant volume was 50% smaller (V100: 42.7 cc vs 83.8 cc; V150: 22.2 cc vs 42.9 cc; V200: 13.1 cc vs 26.0 cc; V300: 5.6 cc vs 12.3 cc). The DC significantly improved to 0.38 from 0.30 for 3- vs 1-tube, respectively (P < .058).
Conclusions: A novel 3-tube endoesophageal HDR technique improved the dose homogeneity and DC in our initial 13 patients. Our initial OS and LC data suggest the potential for an improved therapeutic ratio using a novel 3-tube HDR technique as a component of definitive treatment for stage I–IVA esophageal cancer.