Peripheral T-Cell Lymphomas: Incorporating New Developments in Diagnostics, Prognostication, and Treatment Into Clinical Practice-PART 2: ENKTL, EATL, Indolent T-Cell LDP of the GI Tract, ATLL, and Hepatosplenic T-Cell Lymphoma
In Part 2 of this two-part series, this review covers extranodal natural killer/T-cell lymphoma, enteropathy-associated T-cell lymphoma, indolent T-cell lymphoproliferative disorder of the gastrointestinal tract, adult T-cell leukemia/lymphoma, and hepatosplenic T-cell lymphoma.
Oncology (Williston Park). 32(8):e83-e89.

Figure 1. Epidemiologic Variability of Peripheral T-Cell Lymphomas According to Geographic Location.
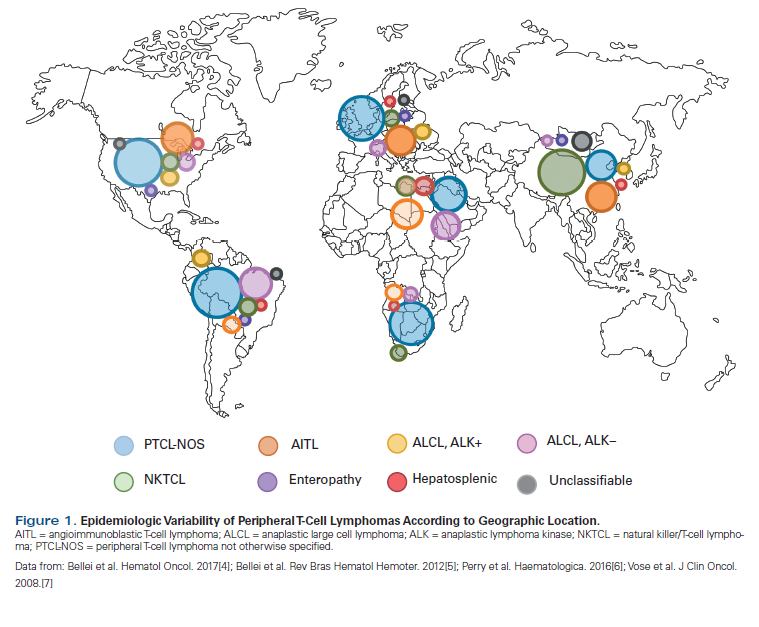
Figure 2. Treatment Algorithm for NK/T-Cell Lymphoma.
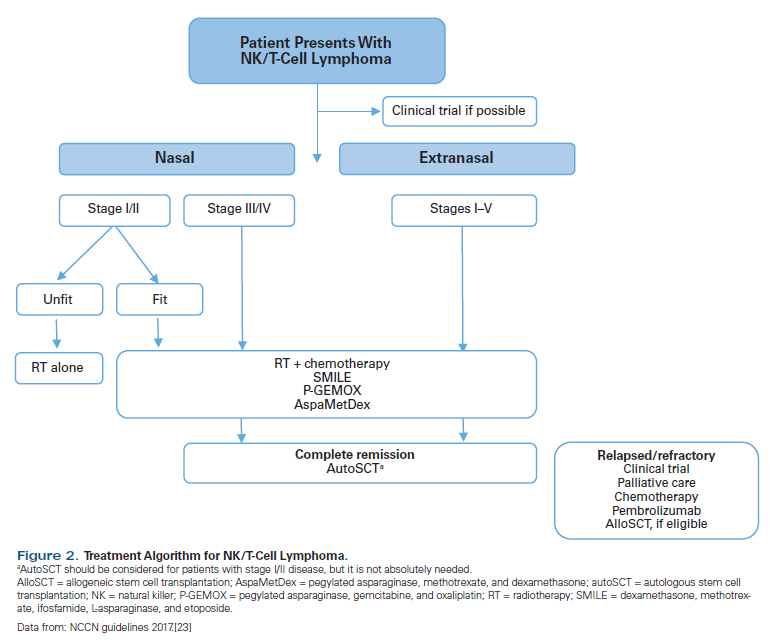
Table 1. Peripheral T-Cell Lymphoma (PTCL): Current World Health Organization Classification
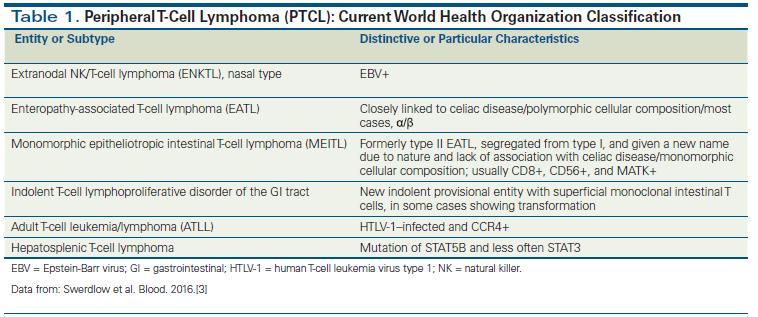
Table 2. Risk Factors Included in the Different Prognostic Indices for NK/T-Cell Lymphoma
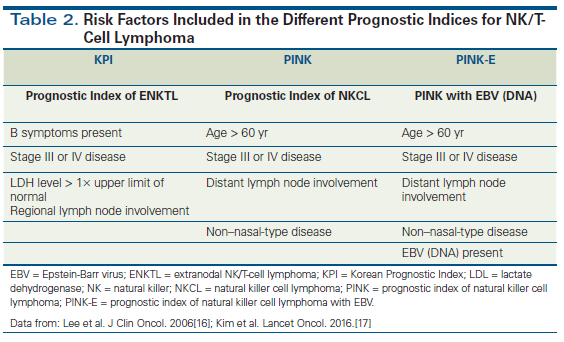
Table 3. Overall Survival by PINK and PINK-E Risk Group
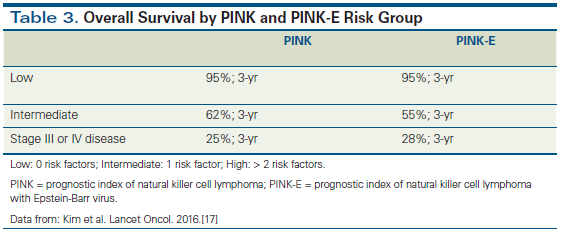
Table 4. PTCL and Genetic Alterations
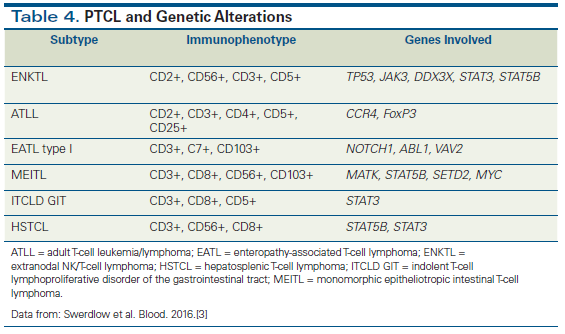
Figure 3. Five-Year Overall Survival of Patients With Adult T-Cell Leukemia/Lymphoma, According to the Clinical Subtype.
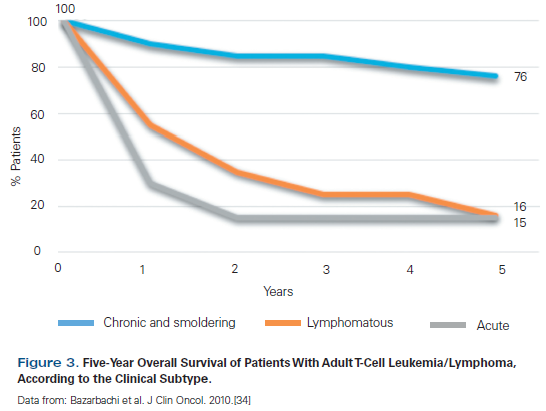
Figure 4. Treatment Algorithm for ATLL.
The World Health Organization classification for peripheral T-cell lymphomas (PTCLs) continues to evolve based on genetic and clinical distinctions of each entity. In Part 1, an overview was provided of PTCL not otherwise specified, follicular T-cell lymphoma, angioimmunoblastic T-cell lymphoma, anaplastic large cell lymphoma (ALCL), and breast implant–associated ALCL. In Part 2, this review is extended to extranodal natural killer (NK)/T-cell lymphoma, enteropathy-associated T-cell lymphoma, indolent T-cell lymphoproliferative disorder of the gastrointestinal tract, adult T-cell leukemia/lymphoma, and hepatosplenic T-cell lymphoma. Each NK/T-cell malignancy has its own signature, requiring knowledge of the appropriate diagnostic, prognostic, and therapeutic considerations when caring for afflicted individuals. Future directions will depend on discoveries that further our understanding of each disease and clinical trials that test the latest treatment options.
Introduction
Peripheral T-cell lymphomas (PTCLs) include a spectrum of mature T-cell and natural killer (NK)-cell neoplasms. PTCLs differ from one another in clinical presentation, pathobiology, prognosis, and therapeutic strategies.[1,2] Their heterogeneity, the challenge of diagnosis, and new knowledge from molecular studies have led to a recent revision of the World Health Organization (WHO) classification for PTCLs.[3]
As described in Part 1, the incidence of PTCLs shows epidemiologic variability worldwide, influenced by factors such as ethnicity, diseases affecting immunity, and virus epidemiology (Figure 1).[4-9]
The current WHO classification for PTCLs includes new subtypes, but due to their low incidence, detailed knowledge of each entity continues to evolve.[3] These subtypes, which will be highlighted in this article, are described in Table 1.[3]
Extranodal NK/T-Cell Lymphoma
NK/T-cell lymphoma is a rare and aggressive disease with a high rate of relapse and poor prognosis.[10] Extranodal NK/T-cell lymphoma (ENKTL) has a male predominance, with a median age at diagnosis of approximately 65 years.[5,9,11] Asia, Central America, and South America demonstrate a higher incidence of NK/T-cell lymphoma.[12] The geographic distribution may in part be explained by the prevalence of Epstein-Barr virus (EBV) and the associated aberrant expression of its receptor, CD21.[8] EBV likely plays a role in the pathogenesis of this cancer, affecting cellular proliferation and the microenvironment, including the expression of programmed death ligand 1 on the malignant cells.[13]
ENKTL has two subtypes. The most common is the nasal type, but extranasal presentations are seen, with different clinical manifestations.[11] The majority of patients with nasal-type ENKTL present with early-stage disease involving the nasal region and the upper aerodigestive tract.[11,14] Symptoms associated with this presentation typically include nasal obstruction, swelling, and bleeding (epistaxis).[11]
Pathologic findings include angiodestruction, necrosis, and ulcers, with the malignant cells embedded in an inflammatory microenvironment. The NK cells express CD2, CD5, cytoplasmic CD3ε, and CD56. These cells are commonly CD8-negative. CD30 is not usually expressed.[11] A spectrum of cytogenetic alterations has been noted without a signature chromosomal translocation. The most common abnormalities are del(6)(q21q25) and i(6)(p10), although it is not clear if these represent primary or progression-associated events.
Clinical staging should include a detailed ear, nose, and throat examination, positron emission tomography–CT imaging, and, in select instances, bone marrow biopsies.[11]
Prognostication using the International Prognostic Index (IPI) is problematic because IPI scores do not correlate with survival. In fact, more than 80% of patients are in the IPI low-risk group, but many still have unfavorable outcomes.[15] The Korean Prognostic Index appears to be a meaningful advance, in particular for patients with nasal presentations.[15] Guidelines from the National Comprehensive Cancer Network recommend the use of the prognostic index of natural killer cell lymphoma (PINK) or PINK-E (incorporating EBV status; Tables 2 and 3).[16-18] Additional prognostic factors include fasting blood glucose level, total protein, and CD30 expression.[15,19]
The treatment for lymphomas originating from NK cells differs from that for other PTCLs, with distinct approaches depending on location (nasal or extranasal) and extent of disease.[20] For the nasal type, radiotherapy is a key component of treatment with curative intent.
In cases of regional disease, an intensive combined-modality approach of sequential or concomitant chemotherapy and radiotherapy is most effective.[10,12,20,21] Chemotherapy alone has been associated with worse outcomes and lower overall survival (OS) when compared with radiotherapy and combined-modality treatment.[12] Regimens containing anthracyclines are not recommended because of inferior outcomes and overexpression of the P-glycoprotein efflux membrane transporter. Regimens containing L-asparaginase or pegylated asparaginase have proved the most successful for patients presenting with advanced-stage NK-cell lymphoma, especially for those with extranasal disease.[10,12,20,21] For patients with early-stage disease (stages I and II) or for those too frail to tolerate chemotherapy, another option is radiotherapy alone.[12,14]
Patients with advanced-stage NK/T-cell lymphoma-either nasal-type or extranasal disease-should be treated with one of the chemotherapy regimens discussed previously. Those who achieve complete response are also candidates for consolidation with autologous stem cell transplantation (autoSCT).[20] For patients with chemotherapy-refractory NK/T-cell lymphoma, autoSCT does not have a clear benefit, and allogeneic SCT (alloSCT) may be a more appropriate therapeutic intervention.[18,22,23]
Pembrolizumab, an anti–programmed death 1 checkpoint inhibitor, has recently been shown to be highly effective for relapsed/refractory cases and has been used after alloSCT with good outcomes (Figure 2).[13,18]
Enteropathy-Associated T-Cell Lymphoma
The involvement of the gastrointestinal (GI) tract is more commonly observed in B-cell non-Hodgkin lymphoma.[24] Enteropathy-associated T-cell lymphomas (EATLs) are rare, typically involve the small intestine, and are divided into two distinct entities in the WHO classification, based on morphology, immunophenotype, and molecular features.[3,6,24] Type I is the most prevalent (~80% to 90% of cases) and has a high prevalence in northern Europe. Type II is now formally designated as monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL) and is more common in individuals of Asian and Hispanic descent.[3,10,25] The majority of patients are diagnosed in their 6th decade.[10,25]
Celiac sprue and the human leukocyte antigen–DQ2/DQ8 phenotype is associated with type I EATL.[6,10,24] Independent of subtype, the malignancy tends to be aggressive.[6] Clinical presentation is characterized by abdominal pain, change in bowel habits, and anorexia.[10] B symptoms are not commonly noted.[26]
EATL type I is typically polymorphic, while MEITL has a monomorphic cellular composition. The characteristic immunophenotype is different for the two subgroups. Most cases of EATL express CD30 and have an α/β T-cell receptor expression, while CD30 expression is uncommon in MEITL cases, which also tend to be more frequently γ/δ-expressing.[3,26] Genetic alterations, including a 9q34 region gain or a 16q21.1 deletion, are frequently detected in EATL patients with celiac disease. Patients without celiac disease frequently have a chromosome 8q gain.[10] Aberrant nuclear p53 protein expression is noted in 75% of cases. Mutations of STAT5B and SETD2 are observed in cases of MEITL of γ/δ origin. Abnormalities affecting MYC signaling are also common in MEITL (Table 4).[3,25]
EATL has a poor prognosis, with a median OS of less than 1 year. [26,27] No standard treatment exists for these patients. Historically, the combination of surgery and anthracycline-based combination chemotherapy, with or without radiotherapy, was employed.[26] Another option for first-line therapy is IVE/MTX (ifosfamide, etoposide, epirubicin/methotrexate), developed by the Scotland and Newcastle Lymphoma Group, which showed an improvement in outcomes when compared with traditional regimens.[25,28] For patients who achieve a complete response, autoSCT is a consideration.[18,25,27]
Indolent T-Cell Lymphoproliferative Disorder of the GI Tract
Indolent T-cell lymphoproliferative disorder (LPD) of the GI tract is an entity recently incorporated into the WHO classification of lymphoid neoplasms.[3] This lymphoma has a male predominance, with a median age at diagnosis of 45 years.[24,27] There is no association with celiac disease, but some patients have a history of Crohn disease.
Presentation with diarrhea is common. At times, there is also abdominal discomfort.[24,29] Fever, weight loss, and night sweats are relatively rare.[24]
The disease usually has an indolent course, without lymphadenopathy or organomegaly. Involvement of the small bowel is most common, although any GI site can be involved and often there are multiple locations.[3] Endoscopic findings are extremely varied and include nodules, ulcers, diverticula, and erosions.[24]
Classically, indolent T-cell LPD of the GI tract is characterized by an infiltration of small, monotonous, and mature lymphocytes involving the lamina propria, with focal infiltration of the muscularis mucosae and submucosa. The mitotic index (or Ki-67 expression) is usually low (eg, Ki-67 expression less than 5%), and EBV is not expressed. CD30+ cells are rare.[24,29]
A limited number of cases have been reported in the literature. Recently published research has demonstrated that progression and transformation are rare.[24,27] Aggressive chemotherapy is of minimal value, and watchful waiting is usually the most appropriate approach.[24,27]
Adult T-Cell Leukemia/Lymphoma
Adult T-cell leukemia/lymphoma (ATLL) is linked to infection with the retrovirus human T-cell leukemia virus type 1 (HTLV-1).[23,30-32] The transmission of HTLV-1 predominantly occurs vertically through exposure to breast milk or blood.[31] The malignant cells show monoclonal integration of the virus.
The epidemiology of the disease reflects the prevalence of HTLV-1 in endemic regions in southwestern Japan, Central America, South America, the Caribbean basin, and western Africa. The incidence is 2.5% among HTLV-1 carriers and is slightly more pronounced among males in their 6th decade, suggesting that infection alone is not sufficient for the development of this malignancy.[32]
Four classic clinical presentations of ATLL have been described: acute, lymphomatous, chronic, and smoldering.[33] The acute presentation is most common and is characterized by lymphocytosis, lymphadenopathy, hepatosplenomegaly, constitutional symptoms, lytic bone lesions, skin rash, and involvement of other organs. Hypercalcemia and elevated lactic dehydrogenase (LDH) levels are frequent laboratory findings. This subtype carries the worst prognosis.[31-33]
The lymphomatous variant is characterized by lymphadenopathy without lymphocytosis. Skin involvement is common and can manifest as an erythematous rash, papules, or nodules.[33]
Patients with the chronic form typically present with skin manifestations, without significant lymphocytosis or lymphadenopathy. Patients with the smoldering subtype have normal peripheral blood counts with skin and/or lung lesions. Enhanced susceptibility to opportunistic infections has been observed in all subtypes and is potentially exacerbated by treatment.[30,33,34]
Generally, ATLL is considered an aggressive disease composed of a pleomorphic lymphoid infiltrate.[31] The “flower cell” or “clover leaf” is the name given to malignant cells with convoluted nuclei that express CD2, CD3, CD4, CD5, and CD25. Associated large transformed cells may be CD30+.[30,31]
The T-cell receptor genes are clonally rearranged. There is no signature cytogenetic abnormality, although generalized genomic mutations (ie, PLCG1, PRKCB, VAV1, IRF4, FYN, CARD11, CCR4, CCR7, and STAT3) and prominent CpG island DNA hypermethylation are noted. The tax gene, a nonstructural gene on the HTLV-1 genome, appears to play a critical role in leukemogenesis, but it is not critical to sustain tumor cell growth. HBZ is one of the few genes consistently overexpressed in most ATLL cases.[30,31] Mutations or deletions involving p53 are also seen and are more common with disease progression.[30]
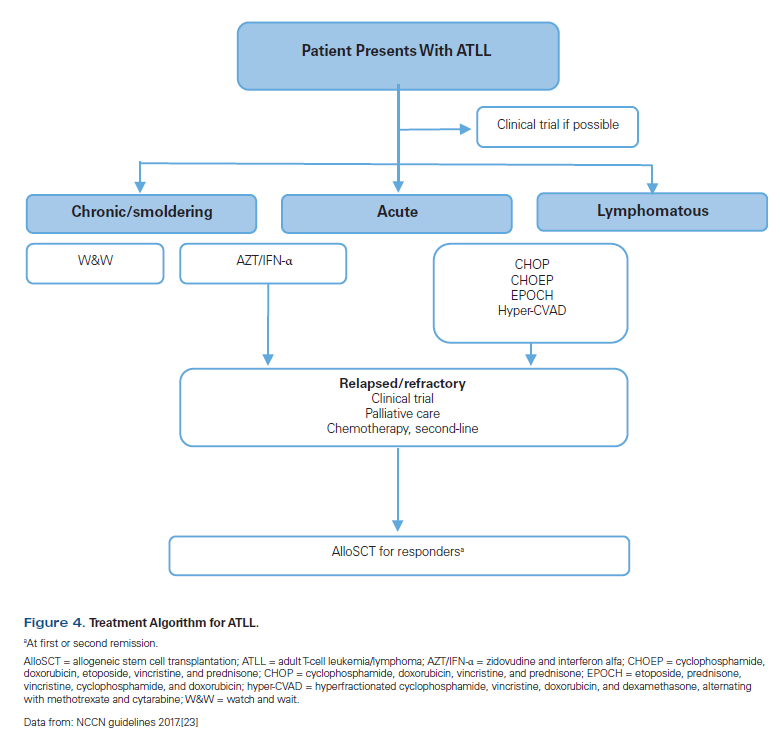
Watchful waiting is recommended for patients who are asymptomatic.[32] Antiretroviral treatment, combining zidovudine (AZT) and interferon alfa (IFN-α), appears to be an option for first-line therapy, in particular for the acute subtype of ATLL. A meta-analysis by Bazarbachi et al evaluated the use of AZT/IFN-α for each subtype of ATLL and its effect on OS (Figure 3).[34] Polychemotherapy containing anthracyclines has historically been used as first-line therapy for patients with the lymphomatous subtype who require treatment, although response rates are low, with frequent relapses and short survival (median, 13 months).[30] Mogamulizumab (anti-CCR4 monoclonal antibody) is approved in Japan for the treatment of relapsed/refractory cases.[31] Alemtuzumab (anti-CD52 monoclonal antibody) also has activity but is associated with severe immunosuppression.[30] AlloSCT should be considered in patients with the acute form who achieve remission, but it is associated with significant morbidity and high relapse rates (Figure 4).[18,30,32]
Hepatosplenic T-Cell Lymphoma
This rare lymphoproliferative disorder, which represents less than 1% of non-Hodgkin lymphomas, predominantly affects young men with a median age of approximately 35 years.[9,18,35] An association with chronic immunosuppression is seen in as many as 20% of individuals.[10,34]
The clinical presentation suggests a very aggressive disease and includes systemic symptoms, hepatosplenomegaly, and pancytopenia.[10] A proliferation of cytotoxic (T1A1+ and granzyme M+) medium-sized T cells is seen infiltrating the sinusoids of the liver, spleen, and bone marrow.[3,8,35]
There are two types of hepatosplenic T-cell lymphoma. The most common type is derived from γ/δ T cells (expressing the Vδ1 chain), and a small percentage derive from α/β T cells.[3,35]
Due to the aggressive nature of the disease, combination chemotherapy (CHOP [cyclophosphamide, doxorubicin, vincristine, and prednisone] or hyper-CVAD [hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone, alternating with methotrexate and cytarabine]) followed by stem cell transplantation is usually recommended.[35] AlloSCT is the preferred front-line consolidation in cases of γ/δ hepatosplenic lymphoma. AutoSCT is reserved for elderly patients or those with significant comorbidities.[36] Unfortunately, most patients do not achieve a complete remission with induction chemotherapy, compromising the stem cell transplantation results.[35]
Conclusion
PTCLs represent a heterogeneous spectrum of malignancies. The low overall incidence of each entity has historically presented a challenge to advancing our knowledge about each disease. It is recommended that the diagnosis be reviewed by an experienced pathologist, in part because a more comprehensive understanding of the molecular, cellular, and phenotypic characterization of the different subtypes has emerged. In most instances, prognosis remains poor, underscoring the importance of having patients participate in clinical trials. In addition, there has been recognition of indolent subtypes that should be observed without immediate intervention. Fortunately, encouraging therapeutic approaches are on the horizon that should have a profound impact on our ability to treat these unique non-Hodgkin lymphomas.
Financial Disclosure:Dr. Zain serves as a consultant for Spectrum Pharmaceuticals, and serves as a consultant and on the speakers bureau for Seattle Genetics. The other authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Moskowitz AJ, Lunning MA, Horwitz SM. How I treat the peripheral T-cell lymphomas. Blood. 2014;123:2636-44.
2. Zain J, Palmer JM, Delioukina M, et al. Allogeneic hematopoietic cell transplant for peripheral T-cell non-Hodgkin lymphoma results in long-term disease control. Leuk Lymphoma. 2011;52:1463-73.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
4. Bellei M, Sabattini E, Pesce EA, et al. Pitfalls and major issues in the histologic diagnosis of peripheral T-cell lymphomas: results of the central review of 573 cases from the T-Cell Project, an international, cooperative study. Hematol Oncol. 2017;35:630-6.
5. Bellei M, Chiattone CS, Luminari S, et al. T-cell lymphomas in South America and Europe. Rev Bras Hematol Hemoter. 2012;34:42-7.
6. Perry AM, Diebold J, Nathwani BN, et al. Non-Hodgkin lymphoma in the developing world: review of 4539 cases from the International Non-Hodgkin Lymphoma Classification Project. Haematologica. 2016;101:1244-50.
7. Vose J, Armitage J, Weisenburger D; International T-Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26:4124-30.
8. Abouyabis AN, Shenoy PJ, Lechowicz MJ, Flowers CR. Incidence and outcomes of the peripheral T-cell lymphoma subtypes in the United States. Leuk Lymphoma. 2008;49:2099-107.
9. Phan A, Veldman R, Lechowicz MJ. T-cell lymphoma epidemiology: the known and unknown. Curr Hematol Malig Rep. 2016;11:492-503.
10. Armitage JO. The aggressive peripheral T-cell lymphomas: 2017. Am J Hematol. 2017;92:706-15.
11. Gill H, Liang RH, Tse E. Extranodal natural-killer/T-cell lymphoma, nasal type. Adv Hematol. 2010;2010:627401.
12. Vargo JA, Patel A, Glaser SM, et al. The impact of the omission or inadequate dosing of radiotherapy in extranodal natural killer T-cell lymphoma, nasal type, in the United States. Cancer. 2017;123:3176-85.
13. Kwong YL, Chan TSY, Tan D, et al. PD1 blockade with pembrolizumab is highly effective in relapsed or refractory NK/T-cell lymphoma failing L-asparaginase. Blood. 2017;129:2437-42.
14. Yang Y, Zhu Y, Cao JZ, et al. Risk-adapted therapy for early-stage extranodal nasal-type NK/T-cell lymphoma: analysis from a multicenter study. Blood. 2015;126:1424-32; quiz 1517.
15. Cai Q, Luo X, Zhang G, et al. New prognostic model for extranodal natural killer/T cell lymphoma, nasal type. Ann Hematol. 2014;93:1541-9.
16. Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006;24:612-8.
17. Kim SJ, Yoon DH, Jaccard A, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol. 2016;17:389-400.
18. Li P, Jiang L, Zhang X, et al. CD30 expression is a novel prognostic indicator in extranodal natural killer/T-cell lymphoma, nasal type. BMC Cancer. 2014;14:890.
19. Horwitz SM, Zelenetz AD, Gordon LI, et al. NCCN guidelines insights: non-Hodgkin’s lymphomas, version 3.2016. J Natl Compr Canc Netw. 2016;14:1067-79.
20. Tse E, Kwong YL. Nasal NK/T-cell lymphoma: RT, CT, or both. Blood. 2015;126:1400-1.
21. Coiffier B, Federico M, Caballero D, et al. Therapeutic options in relapsed or refractory peripheral T-cell lymphoma. Cancer Treat Rev. 2014;40:1080-8.
22. Kharfan-Dabaja MA, Kumar A, Ayala E, et al. Clinical practice recommendations on indication and timing of hematopoietic cell transplantation in mature T cell and NK/T cell lymphomas: an international collaborative effort on behalf of the Guidelines Committee of the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2017;23:1826-38.
23. National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. Chronic lymphocytic leukemia/small lymphocytic lymphoma. Version 5.2018. https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf. Accessed July 3, 2018.
24. Matnani R, Ganapathi KA, Lewis SK, et al. Indolent T- and NK-cell lymphoproliferative disorders of the gastrointestinal tract: a review and update. Hematol Oncol. 2017;35:3-16.
25. Sieniawski MK, Lennard AL. Enteropathy-associated T-cell lymphoma: epidemiology, clinical features, and current treatment strategies. Curr Hematol Malig Rep. 2011;6:231-40.
26. Gentille C, Qin Q, Barbieri A, et al. Use of PEG-asparaginase in monomorphic epitheliotropic intestinal T-cell lymphoma, a disease with diagnostic and therapeutic challenges. Ecancermedicalscience. 2017;11:771.
27. Leventaki V, Manning JT Jr, Luthra R, et al. Indolent peripheral T-cell lymphoma involving the gastrointestinal tract. Hum Pathol. 2014;45:421-6.
28. Sieniawski M, Angamuthu N, Boyd K, et al. Evaluation of enteropathy-associated T-cell lymphoma comparing standard therapies with a novel regimen including autologous stem cell transplantation. Blood. 2010;115:3664-70.
29. Perry AM, Warnke RA, Hu Q, et al. Indolent T-cell lymphoproliferative disease of the gastrointestinal tract. Blood. 2013;122:3599-606.
30. Bazarbachi A, Suarez F, Fields P, Hermine O. How I treat adult T-cell leukemia/lymphoma. Blood. 2011;118:1736-45.
31. Ohshima K. Molecular pathology of adult T-cell leukemia/lymphoma. Oncology. 2015;89(suppl 1):7-15.
32. Katsuya H, Ishitsuka K, Utsunomiya A, et al. Treatment and survival among 1594 patients with ATL. Blood. 2015;126:2570-7.
33. Shimoyama M. Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984-87). Br J Haematol. 1991;79:428-37.
34. Bazarbachi A, Plumelle Y, Carlos Ramos J, et al. Meta-analysis on the use of zidovudine and interferon-alfa in adult T-cell leukemia/lymphoma showing improved survival in the leukemic subtypes. J Clin Oncol. 2010;28:4177-83.
35. Shi Y, Wang E. Hepatosplenic T-cell lymphoma: a clinicopathologic review with an emphasis on diagnostic differentiation from other T-cell/natural killer-cell neoplasms. Arch Pathol Lab Med. 2015;139:1173-80.
36. Kharfan-Dabaja MA, Chavez JC, Khorfan KA, Pinilla-Ibarz J. Clinical and therapeutic implications of the mutational status of IgVH in patients with chronic lymphocytic leukemia. Cancer. 2008;113:897-906.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.