Pattern in Lung Cancer Pathology May Predict Recurrence Risk
Identification of a significant micropapillary component within lung adenocarcinomas predicts a higher risk of relapse following lung-sparing surgery, according to results of a new study.
Identification of a significant micropapillary component within lung adenocarcinomas may predict a higher risk of relapse following lung-sparing surgery, according to results of a study published in the Journal of the National Cancer Institute.
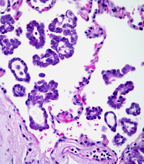
Lung adenocarcinoma with micropapillary component; Image source: Cesar Moran, MD
In lung cancer’s early stages, the current standard treatment is lobectomy with dissection of the hilar and mediastinal lymph nodes. This treatment is quite radical, however, and may be contraindicated in patients with compromised lung function. This has led to some speculation that limited resection of the tumor and the surrounding margins can be as effective in an effort to preserve lung function.
Unfortunately, determining when limited resection is an appropriate treatment has been challenging. In lung adenocarcinoma, the most common histologic subtype of non–small-cell lung cancer, no standardized criteria have been developed that help surgeons decide between lobectomy and limited resection. Small tumors, those less than 2 cm, are thought to be more amenable to this approach. The results of the ongoing CALGB 140503 trial-“A Phase III Randomized Trial of Lobectomy Versus Sublobar Resection for Small (< 2 cm) Peripheral Non–Small-Cell Lung Cancer”-could help resolve this question.
In this report, led by Dr. Prasad Adusumilli of the Sloan-Kettering Memorial Cancer Center, 734 patient samples collected from 1995 through 2009 were included in a study to evaluate the risk of recurrence following lobectomy (n = 476) or limited resection (n = 258). Patient samples were histologically subtyped according to the International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society (IASLC/ATS/ERS) classification criteria. The main outcome assessed was cumulative incidence of recurrence (CIR).
The results showed that the CIR for lobectomy was better than limited resection overall (21.1% vs 15.1%), which was in alignment with previously published data. Next, the researchers attempted to delineate histologic variables that may lead to enhanced risk of recurrence in the limited resection patients. Interestingly, micropapillary component (presence of small papillae) greater than or equal to 5% predicted a high-risk population of patients (34.2% CIR compared with 12.4% in patients with less than 5% micropapillary component). Indeed, when other risk factors such as vascular and lymphatic invasion were excluded, the micropapillary component was found to be an independent risk factor of recurrence following limited resection. Patients undergoing lobectomy showed no elevated risk of recurrence with this same micropapillary component.
Overall, these results suggest that when micropapillary component is greater than or equal to 5%, surgeons should consider lobectomy or limited resection with wider surgical margins, since surgical margins of greater than 1 cm effectively eliminated the risk of recurrence in the study. “It helps surgeons now,” remarked Dr. Adusumilli. “It gives guidance whether to do limited resection or lobectomy, but the problem still is that we can find out this micropapillary only in the histology once the tumor is removed.” Improved prediction of micropapillary component before surgery is critical for patients with small adenocarcinomas. In the future, Dr. Adusumilli and his group hope to identify a biomarker that will help to identify these high-risk features of lung cancer.
In an editorial accompanying the article, Harvey I. Pass, MD, Department of Cardiothoracic Surgery, NYU Langone Medical Center, stated that a lobectomy is still the standard of care and noted one of the limitations of the study. “What we really don’t know is whether the 5% or greater micropapillary component was weighted toward patients who had a wedge resection instead of a segmentectomy because the sublobar resections are lumped together.”
Dr. Pass pointed out that according to the literature, wedge resections have a substantially higher incidence of local recurrence, and that “the data presented [in this study] do not specify whether segmentectomies are equally guilty of a higher cumulative incidence of recurrence.” Dr. Pass emphasized that as a thoracic surgeon, “rather than trying to perform a ‘salvage segmentectomy or lobectomy’, it is my responsibility to get the first operation right, and in 2013, for intentional resections of lung cancer, the only place for a definitive wedge in the intentionally treated lung cancer is in situ carcinoma, leaving all the rest of the lesions for segmentectomy and lobectomy.”