PET/CT Agent Identifies Aggressive Renal Cancers Noninvasively
Screening patients with renal masses with iodine-124-girentuximab had both a high specificity and sensitivity for identifying clear cell renal cell carcinoma, according to the results of a newly published open-label multicenter study.
Screening patients with renal masses with iodine-124-girentuximab had both a high specificity and sensitivity for identifying clear cell renal cell carcinoma, according to the results of a newly published open-label multicenter study.
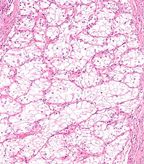
Intermediate magnification micrograph of a clear cell renal cell carcinoma; source: Nephron, Wikimedia Commons
“This is the first example of a prospective multicenter study to demonstrate the ability of PET/CT to identify an aggressive cancer phenotype,” said Chaitanya R. Divgi, MD, director of nuclear medicine/PET at Columbia University Medical Center. “Imaging with PET/CT can replace or guide biopsy, and obviate or guide surgery, in addition to providing a noninvasive way of assessing disease throughout the body.”
Among renal cancers, clear cell renal cell carcinoma (ccRCC) has poor prognosis and a higher potential to become metastatic. Current methods for defining the pathophysiologic characteristics of renal masses include surgery or presurgical renal mass biopsy, both of which have limitations.
Prior research conducted by Divgi and colleagues found that in a group of 26 patients with renal masses, noninvasive PET/CT imaging using the chimeric antibody cG250-or girentuximab-had a high sensitivity and specificity for identifying ccRCC. Based on these results, the researchers designed the Renal Masses: Pivotal Study to Detect Clear Cell Renal Cell Carcinoma with Pre-Surgical PET/CT, or the REDECT study, the results of which were published recently in the Journal of Clinical Oncology.
In the phase III multicenter study, more than 200 patients underwent iodine-124-girentuximab PET/CT and contrast-enhanced CT (CECT) 2 to 4 days prior to scheduled resection of a renal mass. Resulting images from each patient were reviewed by three blinded readers and tumor histology was determined by a blinded central pathologist. Of the cohort, 195 patients had complete data sets.
The average sensitivity for PET/CT was 86.2% compared with 75.5% for CECT (P = .023). Specificity was also higher for PET/CET compared with CECT (85.9% vs 46.8%; P = .005).
“The main finding was a confirmation of our earlier observation that immunoPET with [124I]-girentuximab has utility in identification of the primary clear cell renal cell cancer phenotype,” Divgi said. “While it was a confirmation of our earlier study, it was nevertheless surprising since pivotal multicenter phase III trials do not always confirm data from a pilot single center study.”
According to the researchers, girentuximab may be useful not only in the identification of primary ccRCC, underscoring its ability to be a prognostic biomarker, but also in identification of metastases, with potential as a pharmacodynamic biomarker.
“This information will be tremendously useful in the assessment of renal masses, potentially avoiding unnecessary surgery as well as informing the nature of any surgical procedure,” Divgi said. “In specific instances, this noninvasive imaging procedure may be used to replace or guide biopsy. Moreover, extent of disease evaluation would be very accurate in patients with ccRCC, since the imaging identifies an antigen associated with an aggressive malignant phenotype, with consequent high sensitivity and specificity.”