Potential Brain Cancer Therapy Seen in Affordable Diabetes Drug
Researchers have identified metformin, a drug used to treat diabetes, as a way to activate a key protein that can shut down the continued self-renewal process that keeps producing new glioma cells in glioblastoma patients.
Researchers have identified metformin, a drug used to treat diabetes, as a way to activate a key protein that can shut down the continued self-renewal process that keeps producing new glioma cells in glioblastoma patients. Glioblastoma is the most common and most lethal type of brain tumor. Glioblastomas are generally invasive and aggressive, resulting in mortality after only 2 years for most patients. The study is published in Stem Cells Translational Medicine.
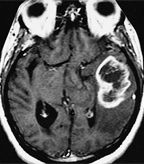
MRI of glioblastoma multiforme
“This is an exciting new concept for glioma and oncology research,” said Michael Ciesielski, PhD, assistant professor of neurosurgery at Roswell Park Institute in Buffalo, New York. Ciesielski emphasized the novel approach of this research. “The vast majority of existing strategies simply target a protein, because it is expressed, and use it to deliver a cytotoxic payload. Here, they have actually triggered the natural function of this particular protein which has led to slowing of cell growth.”
In previous studies, Atsushi Sato, MD, PhD, Chifumi Kitanaka, MD, PhD, and colleagues from Yamagata University in Japan showed a protein called FOXO3 (foxhead box O3), when activated, can cause differentiation of the stem-like glioma cells, inhibiting their ability to initiate a new tumor. The undifferentiated, stem-cell like cells are able to initiate tumors much more readily compared to more differentiated cells. The phosphatidylinositol 3-kinase (PI3K) and mitogen-activated protein kinase (MAPK) pathways are necessary to maintain the stem-like state that initiates glioma cells.
Sato and Kitanaka showed that the FOXO3 protein integrates the signaling from these two pathways. FOXO3 was shown to be sufficient to suppress the tumor-initiating program and induce differentiation. The authors suggested that activators of FOXO3 could be molecular drug targets, tipping the scale towards cell differentiation and preventing tumor initiation. Controlling the cancer stem cell population is seen as a way to control unregulated tumor growth and to increase survival for glioblastoma patients.
In the current study, the researchers found such an activator of FOXO3 in metformin. Metformin was found to activate FOXO3 in vivo and could differentiate the glioma-initiating cells. Because metformin is already a widely used drug and importantly, able to penetrate the blood-brain barrier, it is a “strong candidate for clinical use as a cancer stem/initiating cell-targeting drug against glioblastoma.”
Metformin is a first-line treatment for type II diabetes, used to control glucose blood-levels, particularly for those who are obese or overweight. The drug decreases the amount of glucose absorbed by the body and produced by the liver.
Researchers found a new association between cancer stem cells and glucose metabolism. FOXO3 activation via metformin was sensitive to high extracellular glucose levels.
Ciesielski believes this approach begins to address the concept of treating cancer as a chronic condition-holding the cancer in stasis rather than eradicating the tumor. But Ciesielski is skeptical that a drug such as metformin could kill tumor cells, pointing out that drugs such as metformin “have no cytocidal action, but their effects upon cell cycle and differentiation states could be very important.”
If validated as a potential therapy, combinations of metformin with other therapies are feasible. “It is thought that cancer could be a disease caused by the loss of immune response against early tumor cells. Drugs like metformin could allow an immunopermissive environment to develop in the patient. This would lead to a potential vaccination window of opportunity with cancer vaccines such as SurVaxM,” said Ciesielski. SurVaxM is a cancer vaccine currently being developed for glioblastoma multiforme and anaplastic glioma.
Antitumor effects of metformin have been shown in breast and several other tumors, including inhibition of prostate, breast, and lung cancer stem cells. The current study has linked the activity to specific molecular pathways that can be targeted by other means as well.
“Something that needs to emerge are new drugs that can slow tumor progression but not lead to immunosuppression, which currently is what most anticancer drugs do,” said Ciesielski.