Pre-Transplant FLT3-ITD Detection Confers Relapse/Death Risk in AML
Alternative treatment strategies may be necessary for a high-risk population of patients with acute myeloid leukemia and residual FLT3-ITD.
"At every VAF level, higher intensity conditioning regimens were associated with a reduced risk of relapse and death," according to the study authors.
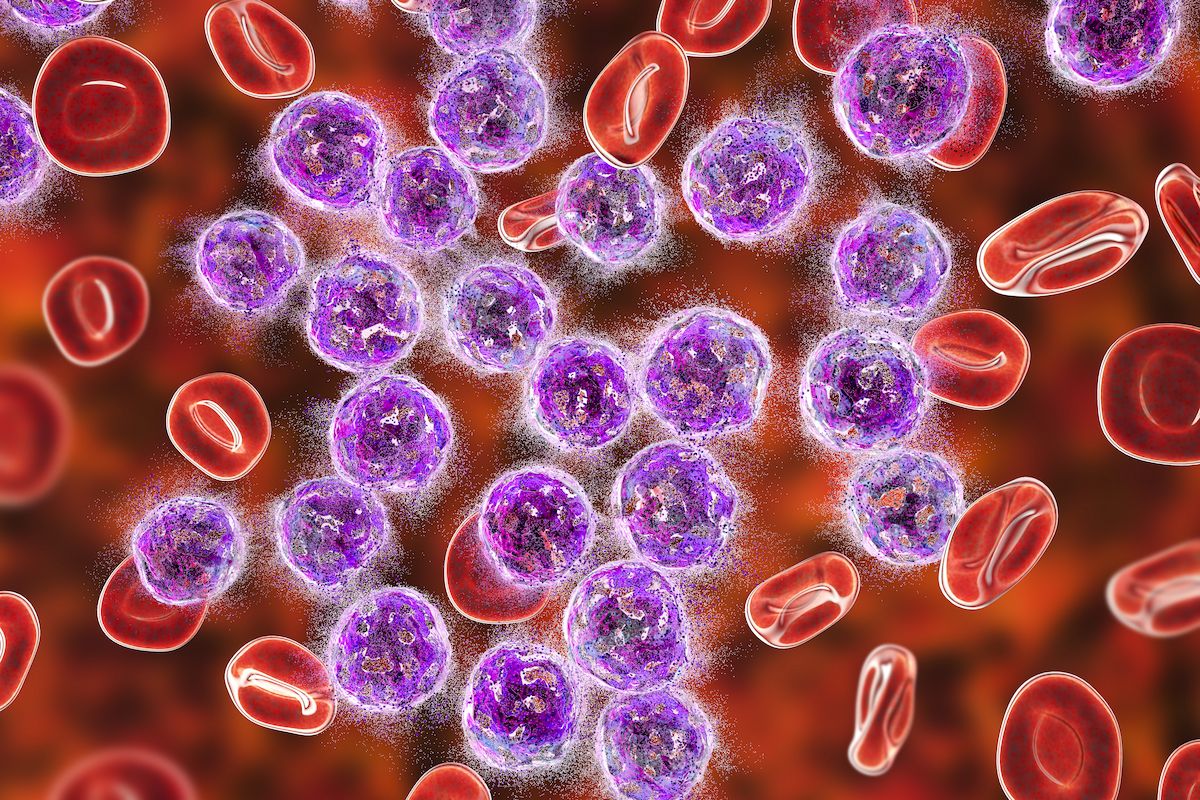
The presence of residual FLT3-internal tandem duplication (ITD) in adult patients with a first complete remission (CR) from acute myeloid leukemia (AML) before allogeneic hematopoietic stem cell (HCT) correlated with a higher risk of relapse and death, according to findings from the Pre-MEASURE study published in JAMA Oncology.
In those who were positive for the FLT3-ITD variant at a variant allele frequency (VAF) cutoff of 0.01% compared with those who weren’t, investigators highlighted a higher rate of relapse (68% vs 26%; P <.001) and a lower rate of overall survival (OS; 24% vs 65%; P <.001) per Invivoscribe (IVS) assessment. Additionally, residual FLT3-ITD was the variable most closely linked to relapse and OS while having a dose-dependent association with disease burden.
Those who underwent treatment with reduced-intensity conditioning without melphalan or nonmyeloablative conditioning therapies were more likely to have a relapse (HR, 2.01; 95% CI, 1.41-2.86) and worse OS (HR, 1.89; 95% CI, 1.41-2.55) compared with those who did receive these treatments. Among patients with a VAF of more than 0 but less than 0.01% who received myeloablative conditioning or reduced-intensity conditioning with melphalan, the risk of relapse was comparable to those without detectable residual FLT3-ITD who were treated with reduced-intensity conditioning without melphalan or nonmyeloablative conditioning.
“At every VAF level, higher intensity conditioning regimens were associated with a reduced risk of relapse and death. The observation that [patients who relapsed] did not have persistent FLT3-ITD detected in remission often had variants in other AML-associated genes detectable in the same pretransplant sample is descriptive but intriguing, highlighting the opportunity for continued refinement of AML measurable residual disease [MRD] testing approaches,” Laura W. Dillon, PhD, FACMG, a staff scientist and director of Laboratory Operations in the Laboratory of Myeloid Malignancies at the National Heart, Lung, and Blood Institute, and coauthors wrote.
In this cohort study, investigators conducted DNA sequencing from the blood of patients 18 years and older with FLT3-ITD AML in first CR who received a transplant between March 2013 and February 2019. IVS, a next-generation sequencing (NGS) kit, was used to detect FLT3-ITD at a minimum VAF of 0.005%; these results were then compared with those reported with a multiplex polymerase chain reaction-based target NGS assay (AMP).
The study’s primary end points were OS and the cumulative rate of relapse. Non–relapse-associated mortality was a competing risk following allogeneic HCT. Investigators used Kaplan-Meier estimations, Cox proportional hazard models, and Fine-Gray models to assess patient outcomes.
Among 537 evaluable patients with sufficient blood samples, the median age was 55.6 years (IQR, 42.9-64.1). After a median follow-up of 35.9 months (IQR, 24.4-59.5), 173 patients had a relapse, and 219 had died. The median time to relapse and death, respectively, was 5.2 months (range, 0.7-52.1) and 10.1 months (range, 0.0-88.4).
Testing with IVS identified 263 FLT3-ITD variants at a median VAF of 0.005% (range, 0.0002%-44%) and a median length of 51 base pairs (range, 5-228). Investigators reported a median of 1 variant (range, 1-15) and a median maximum VAF of 0.01% (range, 0.0003%-44%) among patients with positive findings per IVS testing.
According to the study authors, a potential contributing factor to false-negative FLT3-ITD MRD status results is the categorization of CR status at the time patients underwent MRD testing. Among 240 patients with complete blood count information, the 3-year relapse rate was 57% in those with full CR and a positive result for residual FLT3-ITD variants vs 26% in those who tested negative. Additionally, the OS rate was 32% vs 67% in each respective group.
Reference
Dillon LW, Gui G, Ravindra N, et al. Measurable residual FLT3 internal tandem duplication before allogeneic transplant for acute myeloid leukemia. JAMA Oncol. Published online May 2, 2024. doi:10.1001/jamaoncol.2024.0985