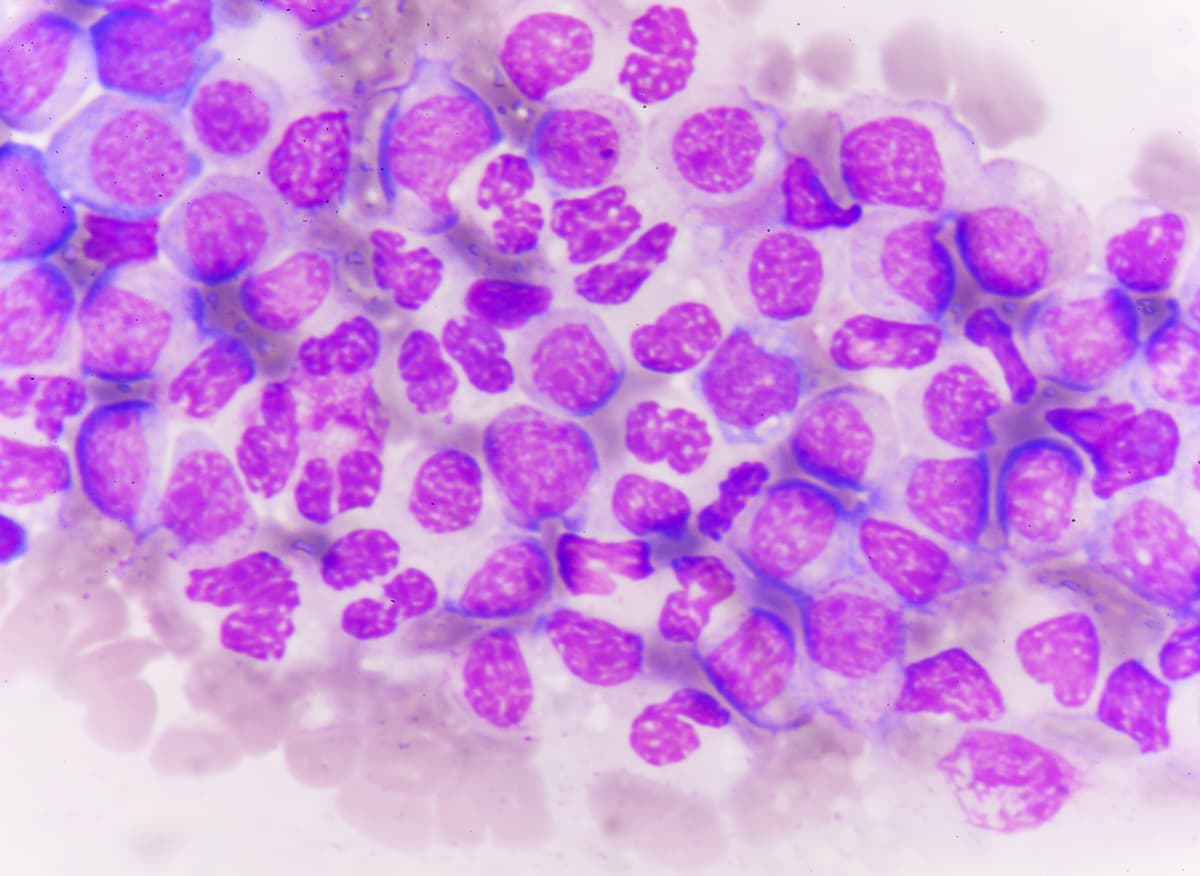
Pre-Transplant Persistent FLT3/NPM1 Variants Signal Worse Outcomes in AML
Further research is necessary to determine whether regular DNA sequence testing for residual disease variants in patients with acute myeloid leukemia can improve outcomes.
The presence of FLT3 internal tandem duplication (ITD) or NPM1 variants in blood at an allele fraction of at least 0.01% prior to hematopoietic cell transplant correlated with increased relapse and worse overall survival (OS) in patients with acute myeloid leukemia (AML) compared with those who did not have said variants, according to findings from a study published in JAMA.
"...these results show that [next-generation sequencing measurable residual disease] testing of the blood of patients with FLT3-ITD and/or NPM1-mutated AML in first remission prior to transplant could identify differential risk between individuals otherwise placed in the same baseline risk classification," according to the authors of a study published in JAMA.
In the discovery cohort, of 64 of 371 patients with persistent NPM1 and/or FLT3-ITD variants in pretransplant remission blood had a higher 3-year post-transplant relapse rate of 59% vs 24% for those without (HR, 3.71; 95% CI, 2.55-5.41; P <.001). Additionally, the 3-year OS rate was 34% vs 66% in each respective group (HR, 2.60; 95% CI, 1.85-3.65; P <.001).
In the validation cohort, 78 of 451 patients with NPM1 and/or FLT3-ITD variants, the 3-year post-transplant relapse rate was 68% vs 21% among those without the persistent variants (HR, 4.32; 95% CI, 2.98-6.26; P <.001). The 3-year OS rate was 39% vs 63% in each respective group (HR, 2.43; 95% CI, 1.71-3.45).
“Although prognostic models based on baseline characteristics can be developed to stratify entire cohorts of patients based on relapse or survival probabilities, these results show that [next-generation sequencing measurable residual disease] testing of the blood of patients with FLT3-ITD and/or NPM1-mutated AML in first remission prior to transplant could identify differential risk between individuals otherwise placed in the same baseline risk classification,” the study authors stated.
Investigators of this retrospective observational study performed DNA sequencing on pre-transplant blood samples from patients who received their first allogeneic hematopoietic cell transplant during first remission of AML associated with variants in NPM1, FLT3, IDH1, IDH2, and KIT. Investigators collected clinical data from patients up to May 2022 through the Center for International Blood and Marrow Transplant Research.
The primary end points of the study were OS and cumulative incidence of relapse with non-relapse mortality as a competing risk. Secondary end points included relapse-free survival (RFS) and non-relapse mortality.
Patients 18 years or older who had a remission blood sample collected within 100 days prior to hematopoietic cell transplant were eligible for inclusion on the study. Patients were also included if they had undergone transplant at least 3 years before the study analysis with relapse and survival data available.
A total of 1075 patients were available for the analysis, 454 of whom received transplant between March 1, 2013, and December 31, 2017 in the discovery cohort and 621 in the validation cohort underwent transplant between January 1, 2018, and February 14, 2019. A total of 822 patients from the discovery and validation cohorts had AML harboring FLT3-ITD and/or NPM1 mutations. The median patient age was 57.1 years and 54% of patients were female.
Investigators indicated that most patient, leukemic, and transplant characteristics were comparable between the discovery and validation cohorts. However, IDH genes at AML diagnosis more frequently appeared in patients from the validation cohort compared with those from the discovery cohort. Additionally, patients in the validation cohort underwent cord blood transplants less frequently than those in the discovery cohort (6% vs 23%).
In the discovery cohort, the 3-year RFS rate was 27% for patients with detectable FLT3-ITD and/or NPM1 variants vs 59% for those who did not have said variants. In the validation cohort, the 3-year RFS rate was 19% vs 59% in each respective patient group.
In the combined discovery and validation cohorts, 94% of patients had undergone flow cytometry as a test for measurable residual disease. Additionally, 7.6% of those testing positive for residual disease following flow cytometry prior to transplant had OS rates that did not significantly differ from those who tested negative (P = .07).
DNA sequencing for residual FLT3-ITD and NPM1 variants in remission blood correlated with statistically significant stratification for post-transplant OS in all molecular subgroups. Additionally, the sequencing also correlated with statistically significant stratification for both younger and older adults, and there were no differences in clinical outcomes based on race.
Based on multivariate analyses, next-generation sequencing of measurable residual disease correlated with both relapse and OS, although receiving reduced-intensity conditioning not containing melphalan also correlated with a higher rate of relapse. In subgroups based on baseline FLT3-ITD and NPM1 variant status, next-generation sequencing of measurable residual disease was significant regardless of the selected variant allele fraction threshold.
Reference
Dillon LW, Gui G, Page KM, et al. DNA sequencing to detect residual disease in adults with acute myeloid leukemia prior to hematopoietic cell transplant. JAMA. 2023;329(9):745–755. doi:10.1001/jama.2023.1363