Primary Hypothyroidism Linked to Reduced Risk of Breast Ca
HOUSTON—Ablation of thyroid hormone function may help prevent the development of breast cancer, according to a study by Massimo Cristo-fanilli, MD, and his colleagues at M.D. Anderson Cancer Center. This work, a retrospective analysis of the incidence of hypothyroidism in breast cancer patients, was published in the Proceedings for the 94th Annual Meeting of the American Association for Cancer Research, scheduled for April 2003 in Toronto; owing to the outbreak of severe acute respiratory syndrome (SARS), the meeting was postponed until July in Washington, DC. The study (abstract 2903) was prompted by reports showing the ability of thyroid hormones to sustain serum-free proliferation of breast cancer cell lines, as well as work that correlated the presence of antithyroid autoantibodies with a better breast cancer prognosis. Thus it seemed reasonable to expect that primary hypothyroidism, which itself is usually an autoimmune syndrome, might reduce the risk of primary breast cancer, as well as ameliorate the course of disease.
HOUSTONAblation of thyroid hormone function may help prevent the development of breast cancer, according to a study by Massimo Cristo-fanilli, MD, and his colleagues at M.D. Anderson Cancer Center. This work, a retrospective analysis of the incidence of hypothyroidism in breast cancer patients, was published in the Proceedings for the 94th Annual Meeting of the American Association for Cancer Research, scheduled for April 2003 in Toronto; owing to the outbreak of severe acute respiratory syndrome (SARS), the meeting was postponed until July in Washington, DC.
The study (abstract 2903) was prompted by reports showing the ability of thyroid hormones to sustain serum-free proliferation of breast cancer cell lines, as well as work that correlated the presence of antithyroid autoantibodies with a better breast cancer prognosis. Thus it seemed reasonable to expect that primary hypothyroidism, which itself is usually an autoimmune syndrome, might reduce the risk of primary breast cancer, as well as ameliorate the course of disease.
This postulate was examined by comparing the frequency of primary hypothyroidism among healthy controls and breast cancer patients. The study population included 1,136 women with newly diagnosed primary breast cancer and 1,090 age- and ethnicity-matched healthy women seen at the breast cancer screening clinic. In the retrospective analysis of case histories, hypothyroidism was considered present only if it was not the result of surgery and if it preceded the breast cancer diagnosis (cases) or the first visit to the screening clinic (controls).
Overall, hypothyroidism prevalence was significantly higher among controls than among breast cancer patients (14.9% vs 7%; P < .001). Cases were 57% less likely than controls to have a previous hypothyroidism diagnosis. These differences were seen in all ethnic groups.
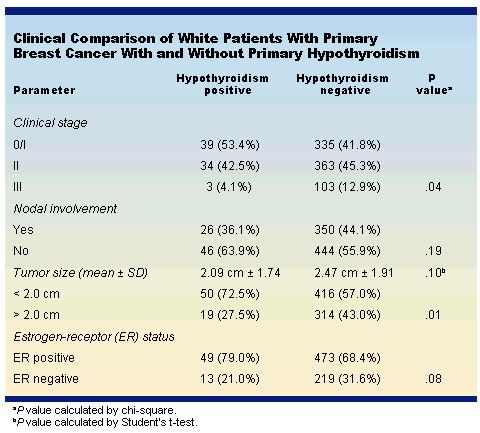
Furthermore, as shown in the Table, invasive breast cancer among patients who were hypothyroidism-positive tended to be less severe. They were likely to have earlier stage disease, smaller tumors, less nodal involvement, and a greater probability of estrogen-receptor (ER)-positive disease. (The table includes only white patients, who comprised the majority of cases analyzed.)
"Even though this is a retrospective analysis, and we are accordingly dealing with relatively small numbers of patients with hypothyroidism, we believe that these data strongly suggest that hypothyroidism exerts a protective effect against developing invasive breast cancer," Dr. Cristofanilli told ONI in an interview.
The investigators are currently planning to undertake a more extensive prospective study to determine the relative prevalence of hypothyroidism among patients with primary breast cancer. Given the more favorable prognosis of ER-positive tumors, he said, they are especially interested in confirming the apparent correlation between this parameter and depressed thyroid function.
"We know that breast cancer cells express significant levels of thyroid receptors, and if we can establish a clinically significant inverse relationship between their activity and the severity of disease, we will have a clear indication that blocking thyroid receptor function has potential therapeutic value in breast cancer treatment," Dr. Cristofanilli said.
This postulate was examined by comparing the frequency of primary hypothyroidism among healthy controls and breast cancer patients. The study population included 1,136 women with newly diagnosed primary breast cancer and 1,090 age- and ethnicity-matched healthy women seen at the breast cancer screening clinic. In the retrospective analysis of case histories, hypothyroidism was considered present only if it was not the result of surgery and if it preceded the breast cancer diagnosis (cases) or the first visit to the screening clinic (controls).
Overall, hypothyroidism prevalence was significantly higher among controls than among breast cancer patients (14.9% vs 7%; P < .001). Cases were 57% less likely than controls to have a previous hypothyroidism diagnosis. These differences were seen in all ethnic groups.
Furthermore, as shown in the Table, invasive breast cancer among patients who were hypothyroidism-positive tended to be less severe. They were likely to have earlier stage disease, smaller tumors, less nodal involvement, and a greater probability of estrogen-receptor (ER)-positive disease. (The table includes only white patients, who comprised the majority of cases analyzed.)
"Even though this is a retrospective analysis, and we are accordingly dealing with relatively small numbers of patients with hypothyroidism, we believe that these data strongly suggest that hypothyroidism exerts a protective effect against developing invasive breast cancer," Dr. Cristofanilli told ONI in an interview.
The investigators are currently planning to undertake a more extensive prospective study to determine the relative prevalence of hypothyroidism among patients with primary breast cancer. Given the more favorable prognosis of ER-positive tumors, he said, they are especially interested in confirming the apparent correlation between this parameter and depressed thyroid function.
"We know that breast cancer cells express significant levels of thyroid receptors, and if we can establish a clinically significant inverse relationship between their activity and the severity of disease, we will have a clear indication that blocking thyroid receptor function has potential therapeutic value in breast cancer treatment," Dr. Cristofanilli said.