Proton therapy needs to prove itself against standard RT
Modeling study calculates that the adoption of proton therapy is possible if it is based on clinical evidence and not market forces.
ABSTRACT: Modeling study calculates that the adoption of proton therapy is possible if it is based on clinical evidence and not market forces.
For devoted proponents of proton-beam therapy, the future looks pretty bright. A field that has been short on clinical data saw multiple studies presented at ASTRO 2009 in support of the technology that is lauded for its lower radiation dose and less toxicity (see "Proton-beam Rx reduces prostate cancer recurrence," January 2010, page 1).
Last month, the first batch of radiation therapists graduated from Ivy Tech Community College in Bloomington, Ind., with certificates to perform proton-beam therapy.
But a major question still looms over this technology: Is proton-beam therapy really better than standard radiotherapy? The Agency for Healthcare Research and Quality (AHRQ) posed this question and others in a 2009 report. The AHRQ technical brief surveyed the current evidence on proton-beam therapy and found that most studies did not include a direct comparison with other radiation-based treatment methods (Visit www.effectivehealthcare.ahrq.gov for the complete report).
Brain tumor treated with proton therapy. Less healthy tissue is exposed to radiation with proton therapy (gray/white area indicates no radiation exposure). Image courtesy of ProCure Training and Development Center and
Sameer Keole, MD
.
One of the coauthors of the AHRQ report, Tomas Dvorak, MD, set out to determine which factors-evidence-based medicine or market forces-will drive the utilization of proton-beam therapy in the future (see Related Reading on page 30).
Dr. Dvorak is a clinical instructor in radiation oncology at Tufts University School of Medicine in Boston. His study coauthors were David E. Wazer, MD, chairman of the department of radiation oncology at Tufts, and Markus Fitzek, MD, MSc, DABR, director of research and development at Midwest Proton Radiotherapy Institute in Bloomington.
Dr. Dvorak discussed the results of his group's current study with Oncology News International. He also offered his perspective on the emerging clinical evidence for proton-beam therapy and whether the technology will truly find a place in the radiation oncology armamentarium.
ONI: Looking at the numbers generated by your study, it would seem that the cost of adopting and deploying proton-beam therapy is quite high. At the present time, do the costs outweigh the benefits?

Dr. Dvorak: You have to put the costs into perspective, and cost is relative. Look at what some of the costs are in medical oncology. What's the cost of putting patients on a maintenance chemotherapy regimen with rituximab (Rituxan) for eight or nine years? As radiation oncologists, we get a bit nervous when people look at our costs out of context.
Yes, the cost is high for proton therapy, but there are two components to the cost. First, there is the capital expenditure for buying the machine and building the facility to house it. That doesn't directly impact spending on healthcare.
Then there is the cost for actual treatment delivered. The fact is that the cost of proton treatment per fraction is higher than the cost of photon treatment per fraction. But using proton therapy in a reasonable fashion may not be that expensive. Based on our study, it only added 15% more on top of the normal budget for radiation therapy delivery.
Whether proton therapy is worth the cost also depends on the disease site. For instance, in pediatric patients with brain tumors or in a woman in her 30s with lymphoma, the consensus is that using proton therapy is meaningful. But is it meaningful for an 80-year-old man with prostate cancer?
At this point, we don't know for whom proton therapy is clinically superior. For our study, we made a judgment based on our clinical understanding of proton therapy and photon therapy to determine which patients we think would benefit. But there are very little actual data to drive these decisions, as demonstrated in our AHRQ study.
ONI: What about the two studies presented at ASTRO 2009 that offered encouraging results for proton-beam therapy in prostate cancer? Investigators at Loma Linda University in California determined that adding a proton boost to conventional radiation reduced the risk of recurrence (abstract 22) while a group from the University of Florida found that proton therapy was well tolerated by prostate cancer patients (abstract 23).
Dr. Dvorak: The [Loma Linda] study is randomized and is a great trial, but it doesn't answer the question of protons vs photons. In this study, they gave a proton boost to photons and compared two different doses. So these results are helpful for deciding whether patients with localized prostate cancer need a higher dose, but they don't tell us whether patients are any better off with proton therapy.
The study does show that the toxicity rate was really low, but again we don't know what the comparable toxicity would be with intensity-modulated radiation therapy (IMRT) using the same schedule.
As for the Florida study, this is a cohort of patients treated purely with protons. It's a prospective trial and that's good, but again there's no comparison. What they've shown us is that they can successfully treat patients with proton therapy, but is it better than standard radiation therapy?
ONI: What is the feasibility of conducting head-to-head trials between proton-beam therapy and photon-beam therapy?
Dr. Dvorak: A lot of people say that they wouldn't feel comfortable randomizing patients to either protons or photons because protons are so superior. Remember, patients at proton therapy centers are preselected. There are only a few centers that offer proton therapy and these patients travel to those centers specifically for that treatment, so the number of patients and physicians who would be willing to participate in a randomized trial is pretty small.
A prospective evaluation with a comparison cohort is not out of the question, as long as patients are being treated appropriately and on protocol. M.D. Anderson [Cancer Center in Houston] has unpublished clinical outcomes that show lower rates of complications with protons vs photons. This led the investigators to open a randomized, phase III trial with Massachusetts General Hospital [in Boston] that compared photon therapy and proton therapy. There are no published results yet, but this effort shows that institutions may be willing to undertake randomized comparisons.
Fact Updated RT guidelines ASTRO has published guidelines for image-guided radiation therapy and stereotactic body radiation therapy (
Int J Radiat Oncol Biol Phys
76:319-325 and 326-332, 2010).
If the M.D. Anderson data demonstrate that treating patients who have advanced lung cancer with protons is better, then you have a huge number of patients who would truly benefit. But if you are treating patients off-protocol, and that's going to be mostly prostate cancer patients, then the likely benefit will be small.
ONI: What about advances in proton therapy technology, such as more targeted beam delivery systems and robotic patient positioning, that will supposedly make the technology more affordable?
Dr. Dvorak: The availability of less expensive technology will go toward capital expenses, but that won't drive down the cost of healthcare delivery, unless the reimbursement decreases as well. However, it will make the technology more accessible.
The more proton therapy centers you have, the more treatment slots you have. But are these slots going to be used appropriately? Are patients going to be enrolled in trials for comparative research or will the centers treat all-comers, and again that will be mostly prostate cancer patients, in order to pay off the cost of the equipment?
ONI: Given the current emphasis on cost-effectiveness in healthcare, what do you see as the future of proton-beam therapy?
Dr. Dvorak: Radiation therapy has made dramatic advances in the past 15 years. It's really not clear at this time whether there is a true difference between protons and photons if you look at dose comparison studies; the region that gets the high curative dose is the same. Actually, [the dose] may be a little bit worse with proton therapy because you are not entirely certain as to where the proton beam stops. Because of that, you need to treat a bigger area with protons than you have to treat with IMRT. So are you overtreating with proton therapy? That's something that new technology may or may not be able to address in the future.
Ultimately, these questions go to the heart of how we in the U.S. decide how we want our healthcare delivered. You have the model of the U.K. and other European countries, where access to technology is tightly controlled. The benefit of that approach is that healthcare doesn't cost as much per person. The downside is that some patients who might potentially benefit from those technologies don't have access to them.
As a physician, if I look purely at the physics of it, protons are better. On that basis alone, I would treat with proton therapy. But on a population basis, that may not be the right decision.
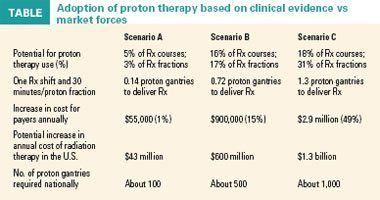
Evidence-based vs market-driven utilization of proton therapy: What could the future hold in the U.S.?
Objective: Estimate the proportion of patients who would be candidates for proton therapy at a tertiary academic center under several adoption scenarios. Financial impact of the scenarios was modeled.
Materials/Methods:
All patients treated in 2009 with radiation therapy were individually evaluated as potential proton therapy candidates. Institution has three linear accelerator particle systems (Linac) and one gamma knife unit. Three utilization scenarios were developed:
Medicare 2008 APC per fraction codes were used to estimate cost; capital expenditure and other charges were not modeled.
Results: In 2007, 1,145 treatment courses using 19,749 treatment fractions were performed on 1,042 patients. Pediatric patients accounted for 2% of all treatments. Clinically reasonable adoption of proton therapy would result in a 17% utilization rate and a 15% cost increase over existing radiotherapy. Market-driven adoption of proton therapy would lead to a 31% utilization rate and a 49% cost increase (see Table above for additional results).
Conclusions: Evidence-based adoption of proton therapy would not significantly increase current radiation therapy outlays. Replacing one Linac gantry with one proton gantry may allow clinically reasonable integration of proton therapy (ASTRO 2009 abstract 1017).