Radical Hysterectomies Show Sexual Toxicity in Early-Stage Cervical Cancer
Radical hysterectomies result in worse symptom experience, body image, menopausal symptoms, sexual worry, sex activity and enjoyment compared with simple hysterectomy in those with early-stage cervical cancer.
Sexual toxicity symptoms seemed to recover over time, allowing for opportunities for early sexual intervention in patients who required radical hysterectomies.
Radical hysterectomy is associated with significantly higher levels of sexual toxicity compared with simple hysterectomy in patients with low-risk, early-stage cervical cancer, according to results from the phase 3 STAGE trial (NCT01658930) presented at the 2023 Annual Global Meeting of the International Gynecologic Cancer Society (IGCS).
As previously reported, the primary end point of pelvic recurrence rate (PRR) at 3 years was 2.52% for simple hysterectomy and 2.17% for radical hysterectomy (95% CI, 2.32%<4%). Investigators could conclude that hysterectomy was non-inferior compared with radical hysterectomy with respect to PRR. The use of adjuvant radiation was less than 10% in both treatment arms.
Results from the sexual health assessment (SHA) showed that patients who received a radical hysterectomy experienced worse sexual vaginal functioning (P <.001 to .02) for up to 24 months, worse desire (P = .001) and arousal (P < .0001) at 3 months, and worse lubrication (P =.003 to .18) and sexual pain (P < .001 to .01) for up to 12 months. Radical hysterectomies also produced sexual dysfunction in the clinical range for up to 6 months (P < .001, .02) and more sexual distress (P = .018) at 3 months compared with simple hysterectomy. There was no change in orgasm or satisfaction.
Sexual toxicity symptoms seemed to recover over time, allowing for opportunities for early sexual intervention in patients who required radical hysterectomies.
“What was striking when we look at the cervical cancer specific module was that radical hysterectomy had worse symptom experience, body image, menopausal symptoms, sexual worry, sex activity, and enjoyment with a small to moderate effect size,” Sarah Ferguson, MD, FRCSC, director of research and professor in the Department of Obstetrics and Gynecology at the University of Toronto, said during the presentation. “What was the most striking was the sexual vaginal functioning subscale. [Patients who received] radical hysterectomy [had] significantly worse [outcomes], and this morbidity lasted up to 2 years.”
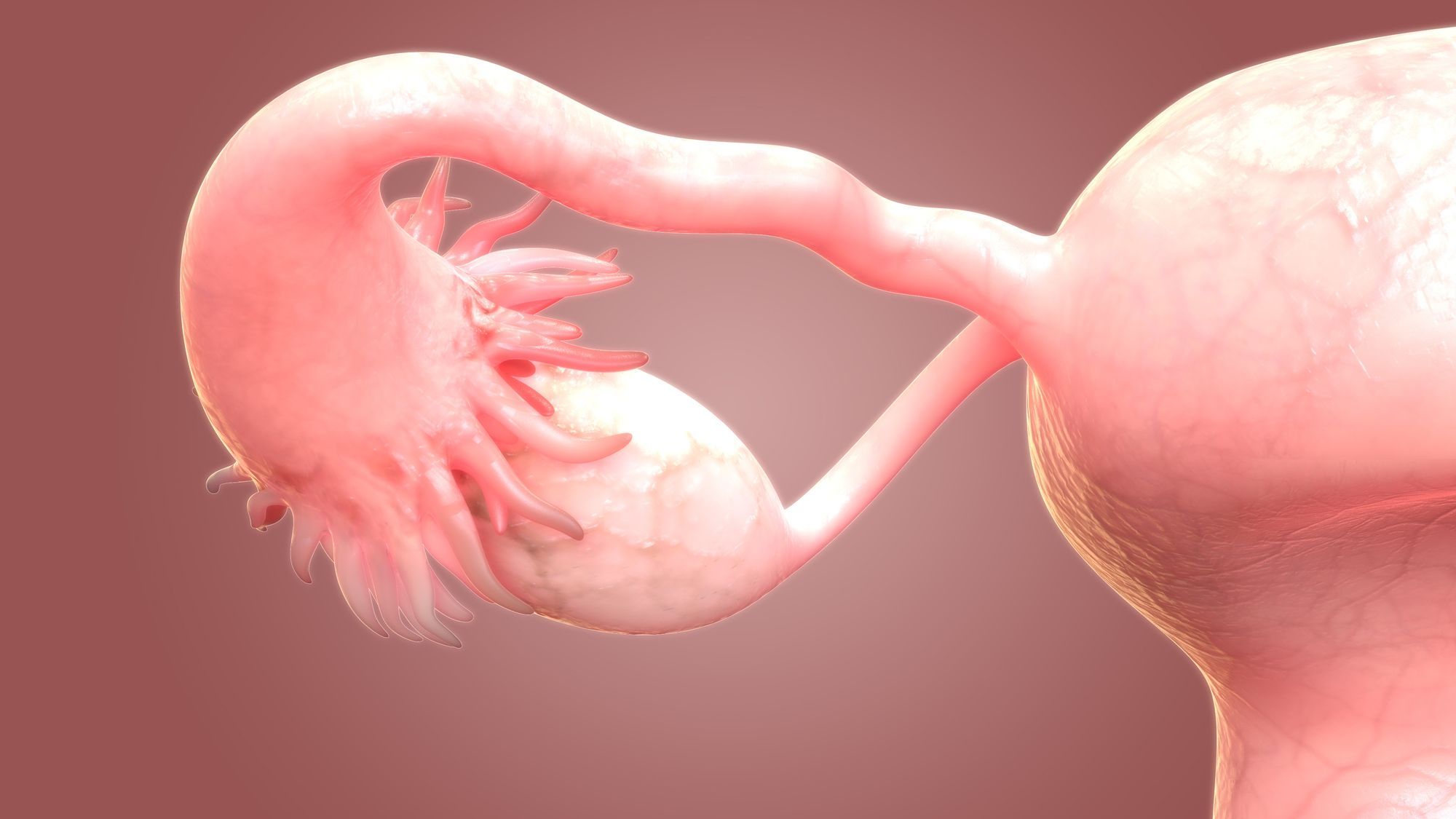
This international, randomized, phase 3 trial included patients with low-risk cervical cancer with a maximum dimension of 20 mm. Patients were randomly assigned 1:1 to receive either radical hysterectomy or simple hysterectomy and were stratified by cooperative group, sentinel node mapping, disease stage (IA2 vs IB2), histological type (squamous vs adenocarcinoma/adenosquamous), and grade of disease (1-2 vs 3 vs non assessable).
Secondary endpoints included patient-reported sexual health and quality of life, which were based on validated questionnaires completed at baseline and at 3, 6, 12, 24, and 36 months following surgery and prior to recurrence. The SHA included 485 patients with a median age of 42 years (range, 24-72) and consisted of the female sexual functioning index (FSFI) and the revised female sexual distress scale (FSDS-R). A total of 85% of patients completed the SHA at baseline, and 65% completed it at 36 months.
The quality-of-life (QOL) assessment included 663 patients with a median age of 44 years (range, 24-77) and was measured through the European Organization for Research and Treatment of Cancer Core Quality of Life questionnaire (EORTC QLQ) and evaluated symptom subscales, including menopausal symptoms. A total of 73% completed the QOL questionnaire at baseline, and 56% completed it at 36 months.
Reference
- Ferguson SE, Plante M, Kwon J, et al. An international randomized phase III trial comparing radical hysterectomy vs simple hysterectomy in patients with low-risk early-stage cervical cancer. Presented at the 2023 Annual Global Meeting of the International Gynecologic Cancer Society (IGCS); Seoul, Korea; November 5-7, 2023. Abstract SE001/1612.