Radiowaves Detect Cancer in Dense Breasts Missed by Mammography
ATLANTA-A novel breast imaging technology that uses radiowaves in the microwave frequency range to detect and locate lesions shows promise in preliminary case reports and will be entering clinical trials, said Allan Malmed, MD, medical director, Northwest Community Hospital Interdisciplinary Breast Center, Arlington Heights, Illinois. Dr. Malmed and his colleagues presented the findings at a poster session of the 102nd Annual Meeting of the American Roentgen Ray Society (abstract 159).
ATLANTAA novel breast imaging technology that uses radiowaves in the microwave frequency range to detect and locate lesions shows promise in preliminary case reports and will be entering clinical trials, said Allan Malmed, MD, medical director, Northwest Community Hospital Interdisciplinary Breast Center, Arlington Heights, Illinois. Dr. Malmed and his colleagues presented the findings at a poster session of the 102nd Annual Meeting of the American Roentgen Ray Society (abstract 159).
X-ray mammography is currently the most effective screening modality, but approximately 10% to 30% of breast cancers go undetected by mammography. "The high number of false negatives may be attributed to the limitations of mammography in assessing dense glandular tissue and regions close to the chest wall or underarm, and in imaging very early stage tumors that do not yet exhibit microcalcifications," Dr. Malmed said.
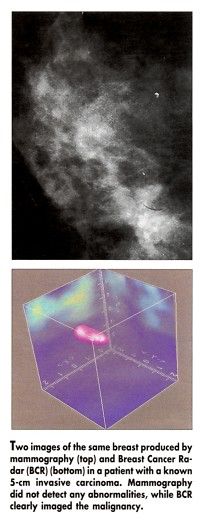
The Breast Cancer Radar (BCR) screening system, which is being developed by Interstitial LLC, Prospect, Illinois, works by detecting differences in water content between malignant and normal breast tissue. Breast tumors contain more water and reflect back the microwave pulses. These signals are analyzed to create a three-dimensional image showing the size and location of the tumor (see Figure).
Dr. Malmed said that the test is simple to perform and takes about 5 minutes. "The patient lies on her stomach on a table that allows her breasts to be scanned by the radiowave signals. There is no compression, and both breasts are imaged at the same time," he said.
BCR was used to detect an infiltrating ductal and lobular carcinoma in the left breast of a 67-year-old woman. The patient had located a mass during self-examination.
The mass was subsequently diagnosed by ultrasound imaging and was palpable, but x-ray mammography 3 months earlier had failed to detect it. The patient’s radiographically dense breast tissue may have lowered the sensitivity of the mammogram, Dr. Malmed said.
To date, the technology has been used to image 22 patients with known cancers or cysts, and the new technology has been able to accurately depict them, Dr. Malmed said. BCR has been used to image cancers as small as 1 cm and cysts as small as 4 mm, and the clinical trials will allow researchers to evaluate the effectiveness of this technique in detecting even smaller cancers.