Real-World Data Confirm Brexu-cel Use in Relapsed/Refractory B-ALL
Consolidative hematopoietic cell transplantation also confers improved progression-free survival among those with relapsed/refractory B-ALL.
"These data also suggest the potential importance of early clearance of [next-generation sequencing]–MRD after brexu-cel on outcomes and support the role of consolidative HCT in appropriate patients," according to the study authors.
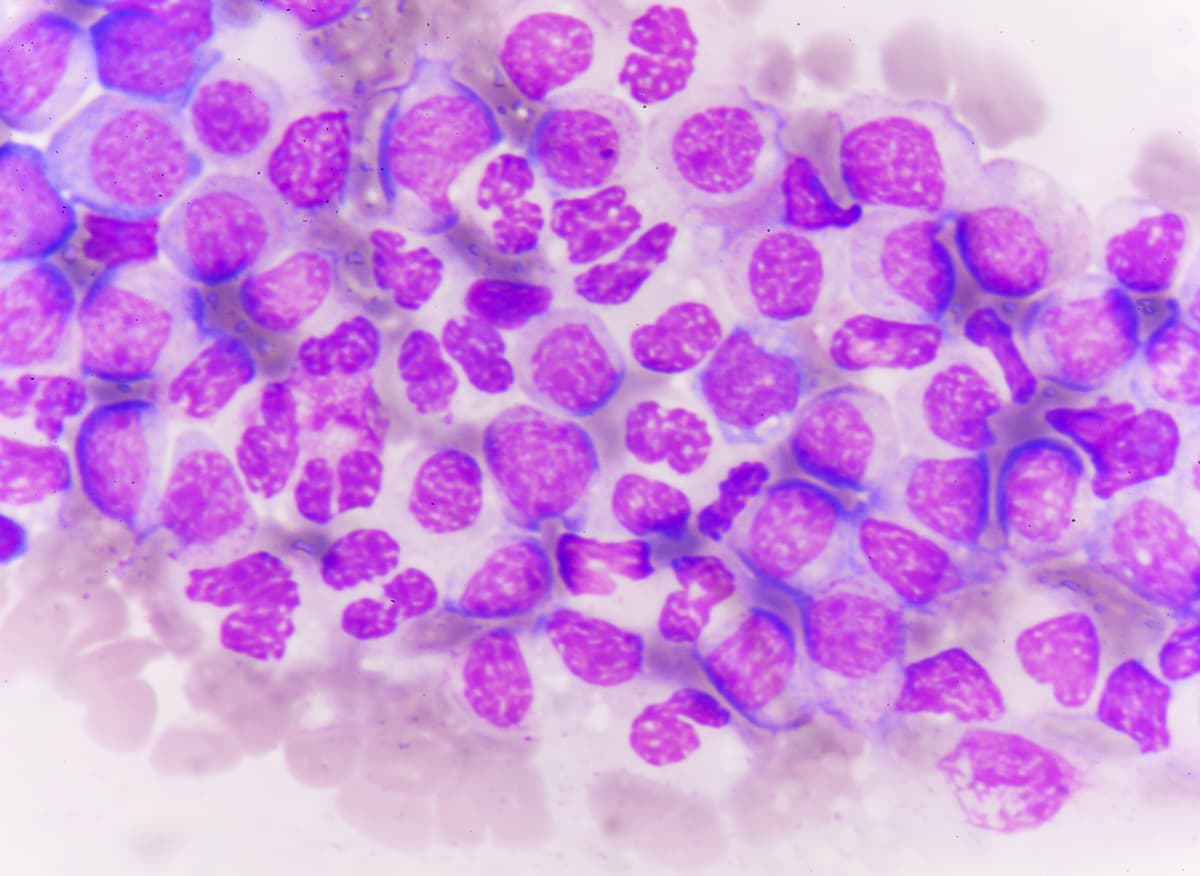
Treatment with brexucabtagene autoleucel (brexu-cel; Tecartus) produced high response and survival rates among patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL), although severe immune effector cell-associated neurotoxicity syndrome (ICANS) and early deaths remain significant clinical concerns, according to retrospective, real-world data published in Journal of Clinical Oncology.
Among evaluable patients, a complete response (CR) or CR or incomplete hematologic recovery (CRi) occurred in 90% (n = 151/168) of patients. Additionally, a minimal residual disease (MRD)–negative CR was reported in 79% (n = 119/151) of patients; MRD-positive CRs and unknown MRD statuses were highlighted in 16% (n = 25/151) and 5% (n = 7/151), respectively.
Of those who achieved a CR with brexu-cel, a relapse occurred in 31% (n = 47/151) with a median time to relapse of 154 days (range, 27-507). The progression-free survival (PFS) rate was 59% (95% CI, 52%-66%) at 6 months and 48% (95% CI, 40%-55%) at 12 months, while data showed an unadjusted median PFS of 9.5 months. The 6-month and 12-month overall survival (OS) rates were 78% (95% CI, 72%-84%) and 63% (95% CI, 55%-60%), respectively; investigators noted that the median OS was not reached.
Overall, 30 patients received consolidative therapy with allogeneic hematopoietic cell transplantation (HCT) at a median 99 days (range, 45-234) between brexu-cel infusion and initiation of HCT. When censoring for HCT following brexu-cel administration, the 12-month PFS and OS rates were 46% (95% CI, 38%-55%) and 63% (95% CI, 54%-71%), respectively.
“To our knowledge, this large, multi-institutional analysis is the first to describe clinical outcomes after brexu-cel delivered as a standard-of-care therapy in adults with [relapsed/refractory] B-ALL. Our data confirm the excellent response rates, CAR T-cell–mediated toxicities, and impressive survival seen in the ZUMA-3 trial [NCT02614066],” Gregory W. Roloff, MD, an assistant professor of medicine at University of Chicago Medicine, and coauthors wrote in the publication. “These data also suggest the potential importance of early clearance of [next-generation sequencing]–MRD after brexu-cel on outcomes and support the role of consolidative HCT in appropriate patients.”
Investigators formed the Real-World Outcomes Collaborative of CAR T in Adult ALL (ROCCA) consortium to evaluate the real-world responses, toxicities, and factors associated with prolonged PFS when using brexu-cel for adult patients with relapsed/refractory B-ALL. Patients 18 years and older who received treatment with brexu-cel from October 2021 to August 2023 were included in the analysis. Those who underwent treatment with the agent as part of a clinical trial or expanded access protocol were not included.
Of 204 patients who underwent apheresis, 189 received an infusion of brexu-cel at the standard dose of 1.0 x 106 cells/kg. The median patient age was 46 years (range, 18-81). Additionally, most patients were non-Hispanic White (55%), had Philadelphia chromosome (Ph)–negative or other disease (53%), active disease with more than 5% blasts (50%), and a pre-apheresis bone marrow blast of lower than 25% (53%). Additionally, patients received a median of 4 (range, 2-12) prior lines of therapy, and most had received prior blinatumomab (Blincyto; 59%).
Based on univariate analysis, factors including Ph-positive disease, prior HCT, and MRD-negative response following brexu-cel conferred an improved PFS (P <.1). Factors associated with worse PFS included prior inotuzumab ozogamicin (Besponsa), marrow blasts of 25% to 74%, and bridging therapy (P <.1).
Multivariate analysis highlighted that prior HCT (HR, 0.41; 95% CI, 0.22-0.76; P = .004) and post-remission consolidative transplant (HR, 0.34; 95% CI, 0.14-0.85; P = .02) conferred improvements in PFS. Additionally, prior receipt of inotuzumab ozogamicin correlated with worse PFS outcomes (HR, 1.75; 95% CI, 1.04-2.94).
Any-grade cytokine release syndrome (CRS) occurred in 84% of patients, with grade 1/2 events occurring in 73% and grade 3/4 toxicity affecting 11%. The median onset to CRS was 5 days (IQR, 4-7).
Any-grade ICANS was reported in 56% of patients; grade 1/2 events affected 24%, and grade 3/4 events were highlighted in 31%. Data showed that the median time to ICANS onset was 7 days (IQR, 6-9). Grade 3/4 CRS conferred higher disease burden at the time of apheresis, although grade 3/4 ICANS did not (P = .006).
Common toxicity management strategies included the use of tocilizumab (Actemra; 82%), steroids (77%), and anakinra (Kineret; 28%). The median length of hospitalization was 15 days (range, 0-95). Overall, 34% (n = 64) of patients died in the study, and 13% (n = 25) died with the absence of progressive leukemia. Additionally, 5.3% (n = 10) of these patients died due to toxicity and/or infection within the first 4 weeks of treatment.
Reference
Roloff GW, Aldoss I, Kopmar NE, et al. Outcomes after brexucabtagene autoleucel administered as a standard therapy for adults with relapsed/refractory B-cell ALL. J Clin Oncol. Published online October 17, 2024. doi:10.1200/JCO.24.00321.