Recap: US Physician PARADIGM Study Informs Decision-Making in Locally Advanced/Metastatic Urothelial Carcinoma
Shilpa Gupta, MD, and Vinit Makkar, MD, discuss the treatment patterns and disease management of locally advanced/metastatic urothelial carcinoma, with a focus on data from the US physician-based PARADIGM study.
Prior research has shown that between 40% and 65% of patients with locally advanced or metastatic urothelial carcinoma (la/mUC) do not receive frontline systemic therapy. Of those who do, around 40% do not receive standard-of-care platinum-based chemotherapy.1,2
With evidence supporting the use of immunotherapy as frontline maintenance following chemotherapy and an aging population of patients to consider, the treatment landscape for urothelial carcinoma is rapidly changing. As part of the CancerNetwork® Between The Lines series, Shilpa Gupta, MD, director of genitourinary medical oncology at the Taussig Cancer Institute and co-leader of the Genitourinary Oncology Program at the Cleveland Clinic, and Vinit Makkar, MD, medical director at Hillcrest Hospital, a regional Cleveland Clinic site, evaluated real-world factors associated with utilization of frontline systemic therapy and maintenance. To do this, they examined results of the PARADIGM study regarding disease management, frontline therapy choice, practice patterns, and decision making in urothelial carcinoma.
Patient Characteristics and Treatment Patterns
To begin, Gupta and Makkar outlined basic patient characteristics and treatment options for urothelial carcinoma. According to Makkar, the typical patient is in their 60s or 70s, although some patients may even be in their 90s.
“The typical discussion with our patients focuses around whether or not they’re candidates for chemotherapy, and particularly whether they’re candidates for platinum-based chemotherapy,” Makkar said. He added that immunotherapy now represents another treatment option, although pairing immunotherapy with chemotherapy, which is helpful in other malignancies such as lung cancer, does not translate into effective treatment for urothelial carcinoma. Rather, immunotherapy in recent years has been used sequentially following chemotherapy.
“Depending upon performance status or patient wishes…immunotherapy is sometimes moved up into the frontline setting instead of chemotherapy,” said Makkar. “But often for metastatic disease, we are routinely talking with patients, especially those who get chemotherapy, about the use of maintenance immunotherapy afterward.”
Unmet Needs in Urothelial Carcinoma
Gupta acknowledged that major progress has been made in the treatment of urothelial carcinoma in recent years. In particular, data from the JAVELIN Bladder 100 trial (NCT02603432) paved the way for use of immunotherapy in the disease, she said. In that study, maintenance therapy with avelumab (Bavencio) paired with best supportive care, compared with best supportive care alone, prolonged the overall survival of patients with urothelial cancer who did not have disease progression with frontline chemotherapy. Those assigned to avelumab experienced a 7-month improvement in survival (21.4 vs 14.3 months; HR, 0.69; 95% CI, 0.56-0.86; P = .001).3
“We have moved so far along with immunotherapy, [which was initially approved] for platinum-refractory disease4-6 and has now moved into non–muscle-invasive bladder cancer. We’re doing a lot of trials in the neoadjuvant setting. Sequential use of immunotherapy maintenance has moved the needle,” said Gupta.
“This is a real breakthrough,” Makkar replied. “Previously, for patients with la/mUC, the duration of benefit from platinum-based chemotherapy was good, but finite. And we know that people with visceral metastases or nonnodal metastases, especially, have worse prognoses.” The fact that immunotherapy could add an average of 4 to 6 months of survival for patients, he went on, was “groundbreaking.”
A major unmet need, Makkar continued, is determining which treatments in an ever-expanding range of options would be most helpful.
“In the first-line setting, we have standard chemotherapy and, in certain circumstances, immunotherapy or checkpoint inhibitors,” Makkar said. “As we get to the second-line setting, we still have checkpoint inhibitors, and we have sacituzumab govitecan [Trodelvy], enfortumab vedotin [Padcev], and targeted therapy.”
In lung cancer, for example, clinicians can use PD-L1 expression as a biomarker for decision making, said Makkar, but the same is not necessarily true in urothelial carcinoma.
“I think this would be very valuable for our urothelial cancer patients, too, just to know…which treatments are the best for which patients and at what point in their [therapy] course.”
Decision-Making in Urothelial Carcinoma
Next, the conversation turned to the results from the PARADIGM study that were presented at the 2022 Genitourinary Cancers Symposium,1 which focused on determining how real-world clinicians have handled la/mUC in recent years. Gupta and colleagues conducted a literature review from January 2018 to March 2021 and used the results to find clinicians to interview about first-line management of la/mUC. One hundred and fifty oncologists’ practice patterns in managing urothelial carcinoma were evaluated by way of 35-minute online surveys
The investigators reported a “relatively low utilization” of frontline systemic therapy, with up to two-thirds of patients with la/mUC not treated.
“[A total of] 63% of providers were in the community setting. [These data] provide us with real-world treatment patterns for patients with urothelial carcinoma,” said Gupta. “We asked oncologists how much [various] factors impact their treatment prescription, like overall survival, progression-free survival, response rates, disease control rates, duration of response, and toxicity. And then there are other considerations, such as other barriers which are beyond control, like institutional guidelines or pathways; frequency of visits; patient co-pays; or any other reasons.”
With these things in mind, Gupta asked Makkar to describe the “most important driver” he considered when prescribing frontline or maintenance treatment. Makkar responded that he makes his decisions based on individual patient characteristics and needs. In younger, more fit patients, he said survival should be the goal, whereas in older, less fit patients, disease management and symptom burden control were more important.
“If the patient with la/mUC is a person with fewer comorbidities, the goal should be survival,” Makkar said. “On the other hand, if they are older, have a poor performance status, or a number of other medical comorbidities, then the goals change. Survival is always important, but perhaps the most important thing in this setting is disease control rate and symptom control.”
Makkar emphasized that in younger patients, particularly those with good kidney function, he tended to use cisplatin, whereas for platinum-eligible patients who were considered borderline, he considered split-dose cisplatin.
“[For those who] have poor renal function or who [may be] at high risk for toxicity, I would choose alternate therapy instead of a platinum-based chemotherapy as the first line of treatment,” Makkar said.
“I think many times, when we are seeing patients, that’s also what we hit upon: The therapy should not be more toxic than the benefit,” Gupta replied. Still, she stressed, clinicians should offer platinum-based therapies whenever possible.
Gupta often uses avelumab as a maintenance immunotherapy, she went on,
because immune-related adverse events tend to be manageable. Gupta added that she had used pembrolizumab (Keytruda) as a maintenance therapy in situations when a patient could not receive treatment every 2 weeks.
Overcoming Barriers to Administration
Gupta said the clinician survey indicated that poor performance status (77%), patient preference (74%), advanced age (69%), toxicity concerns (55%), and limited social and caregiver support (52%) were all factors that might make care providers decide against prescribing first-line systemic therapy. Regarding immunotherapy maintenance in those without progression on frontline chemotherapy, patient refusal (68%), poor performance status (53%), tolerability concerns (43%), high cost of treatment (27%), and issues with reimbursement (27%) were the top 5 reasons for nonutilization.
“When you will not offer any systemic therapy, not even immunotherapy, the patient is probably in bad shape,” Gupta said. Makkar echoed this sentiment, but added that the patient’s geographical location may also play a role.
“I also believe that practice patterns differ depending upon what part of the country [you’re in], whether it’s urban, suburban, or more of a rural setting,” said Makkar. “I suspect that people in rural areas may be less apt to get first-line therapy. In suburban and urban areas where the care is more readily available and accessible, that’s where you’ll find more people getting frontline therapy.”
Gupta pointed to other results from PARADIGM that were read out at the 2022 American Society of Clinical Oncology Annual Meeting. Only a small minority of patients mentioned by clinicians in the survey were offered nonplatinum chemotherapy, Gupta pointed out, which was in keeping with guidelines that emphasize platinum-based chemotherapy as the standard of care.
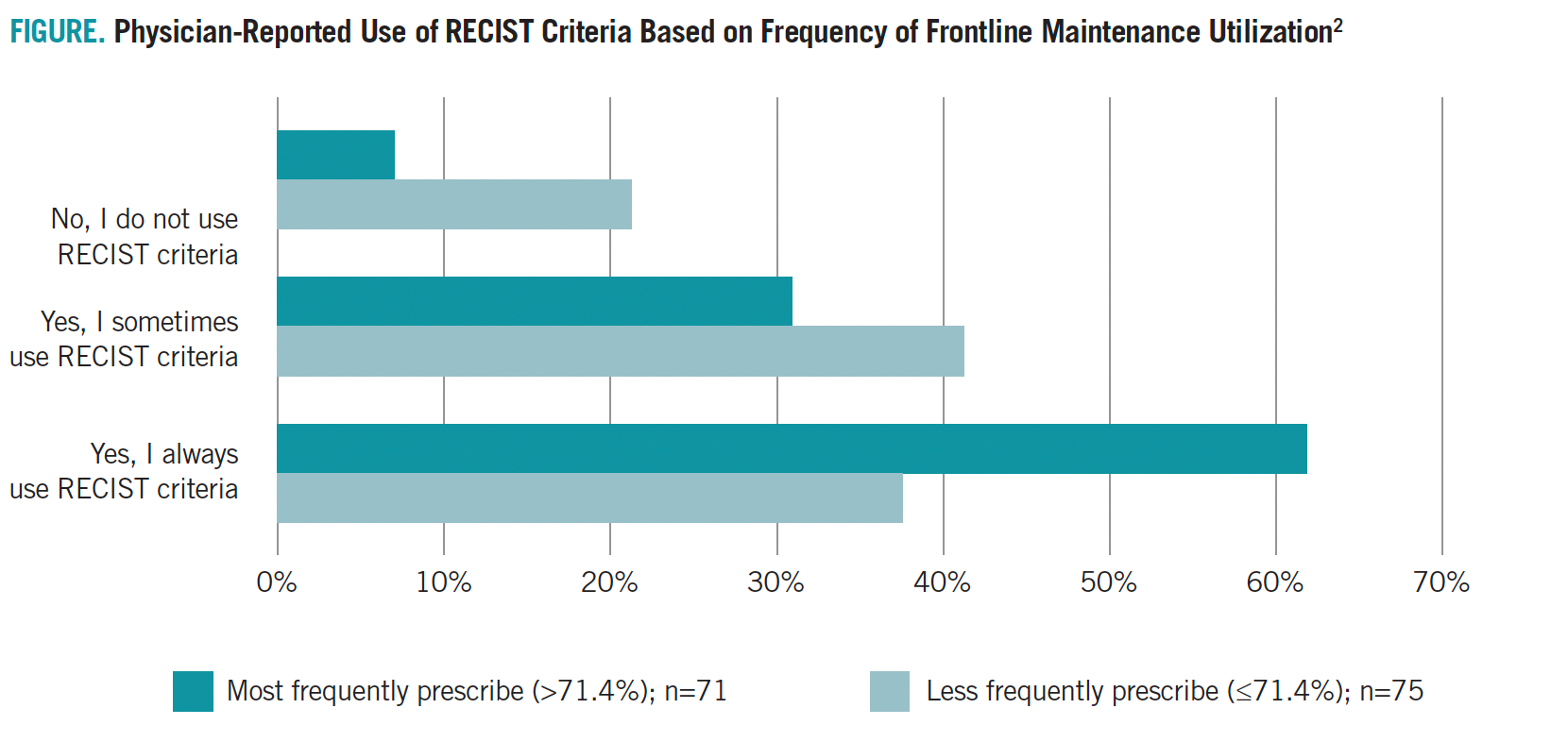
The conversation then turned to the observation that, according to PARADIGM part 2, oncologists who used RECIST criteria to assess treatment
response were more likely to use first-line therapies (FIGURE).2
FIGURE. Physician-Reported Use of RECIST Criteria Based on Frequency of Frontline Maintenance Utilization
“It is well known that therapies are underutilized in cancers like urothelial carcinoma compared with [other malignancies like] breast cancer, where patients are willing to take on more and more therapy. We need to do a better job for these patients,” Gupta said.
“It’s astonishing that in the database, first-line therapy was underutilized,” Makkar said. “The patient’s voice does matter,” he added. “People want to live longer. They may be facing an incurable disease, but more and more, cancer is becoming more of a chronic disease.”
Ultimately, the experts agreed that their consensus on chemotherapy for bladder cancer has come full circle in recent years.
“Back in the [early] 2000s, people weren’t all that excited about chemotherapy for bladder cancer, but now you can see what it can do,” Makkar said.
“[We] became very excited about immunotherapy and now we’ve gone back to carboplatin knowing that it is doable and better. It’s important to get this message out: Chemotherapy is not really bad,” Gupta said.
A major challenge for the future, Gupta went on, is not necessarily getting approval for new therapies but rather getting oncologists to take up current best practices. “There’s still a long way to go to ensure we can be better at utilization,” she said.
“A part of this ought to be community outreach,” said Makkar. “Part of that is with the physicians, but then the other part is in getting the word out to the community that chemotherapy really does work and it can make a difference in someone’s life.”
References
- Gupta S, Su C, Bhanegaonkar A, et al. Disease management and frontline treatment of locally advanced or metastatic urothelial (la/mUC) carcinoma: The U.S. physician PARADIGM study. J Clin Oncol. 2022;40(suppl 6):456. doi:10.1200/JCO.2022.40.6_suppl.456
- Liu F, Costantino H, Ike C, et al. Evaluating oncologists’ practice patterns and decision-making in locally advanced or metastatic urothelial carcinoma (la/mUC): the U.S. physician PARADIGM study (part 2). J Clin Oncol. 2022;40(suppl 16):abstr 4595. doi:10.1200/JCO.2022.40.16_suppl.4595
- Powles T, Park SH, Voog E, et al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218-1230. doi:10.1056/NEJMoa2002788
- Pembrolizumab (Keytruda): advanced or metastatic urothelial carcinoma. FDA. May 19, 2017. Accessed July 13, 2022. https://bit.ly/2oIgNOd
- FDA grants accelerated approval to avelumab for urothelial carcinoma. FDA. May 9, 2017. Accessed July 13, 2022. https://bit.ly/3PlgEYB
- Durvalumab (Imfinzi). FDA. May 1, 2017. Accessed July 13, 2022. https://bit.ly/3RuB3M4