Researchers Predict ADH Patients at Low Risk for Breast Cancer
Researchers have identified a group of women with atypical ductal hyperplasia found on biopsy who should be considered to be at low risk for developing cancer.
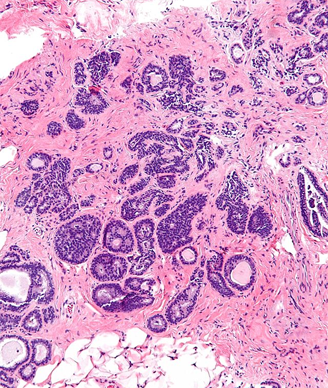
Intermediate magnification micrograph of atypical ductal hyperplasia. Copyright 2011 Nephron.
Researchers have identified a group of women with atypical ductal hyperplasia found on core needle biopsy who should be considered to be at low risk for disease upgrade. These women should be considered for prevention therapy and surveillance rather than undergoing surgical excision, according to Alvaro Pena, MD, of the Mayo Clinic, Rochester, Minn., who presented the results of a retrospective analysis (Abstract 3) at the 2014 American Society of Clinical Oncology (ASCO) Breast Cancer Symposium.
Atypical ductal hyperplasia is found in between 8% to 17% of all core needle biopsies. ADH is a high-risk lesion increasing a woman’s long-term risk for breast cancer.
In this analysis, Pena and colleagues attempted to create a model using clinical, mammographic, and histologic features to identify a subgroup of women with atypical ductal hyperplasia found on core needle biopsy who may be at low risk of cancer upgrade.
They evaluated all cases of atypical ductal hyperplasia diagnosed with core needle biopsy with subsequent surgical excision at the breast surgical practice of Mayo Clinic between June 2005 and June 2013. They also collected data on age, BMI, family history of breast cancer, and prior history of contralateral breast cancer.
The mean age of patients was 58 years. The researchers were able to identify 399 biopsies. At surgical excision, 55 cases of ductal carcinoma in situ and nine cases of invasive cancer were identified. The overall rate of upgrade was 16%.
In terms of clinical features, the researchers did not find any clinical features associated with a higher risk for disease upgrade. In contrast there were several radiologic features that were significantly associated with upgrade to cancer including larger lesion size (P = .0002), smaller needle gauge (P = .002), and cases with removal of less than 90% of the lesion (P < .0001). Breast density, lesion morphology, type of biopsy device, and type of imaging guidance were not associated with an increased risk for disease upgrade.
Similarly, several pathologic features were associated with increased risk for upgrade including the number of foci with atypical ductal hyperplasia (P < .0001), micropapillary with atypical ductal hyperplasia (P = .005), and individual cell necrosis (P < .0001).
The researchers conducted a multivariate analysis and found three features with the highest association with disease upgrade. Patients with less than 50% of their lesion removed had a fourfold increased risk for disease upgrade (OR = 3.8; 95% CI, 1.7-8.6). Patients with two to three foci on core biopsy had a twofold increased risk for upgrade (OR = 2.1; 95% CI, 0.9-4.9), and those with three or more had almost a fourfold increased