Strategies for Addressing Cancer Patients’ Complaints of Fatigue
Cancer-related fatigue is a common, albeit complex, symptom experienced by many cancer patients. Identification of fatigue and assessment of its severity should be a part of routine office care and can be performed using simple, one-question screening tools.
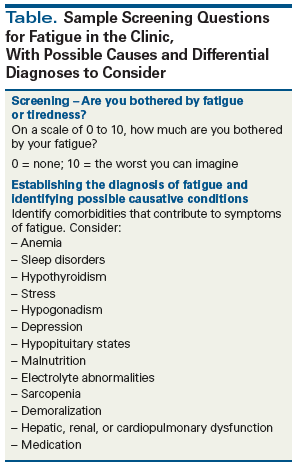
Table. Sample Screening Questions for Fatigue in the Clinic, With Possible Causes and Differential Diagnoses to Consider
Cancer-related fatigue is a complex and common symptom for cancer patients. This article reviews important topics that oncology practitioners should know to better manage fatigue in this patient population. Our discussion includes identification and assessment of fatigue severity, as well as screening for comorbid conditions that may be contributing to an individual patient’s fatigue. Finally, we review nonpharmacologic and pharmacologic interventions for the treatment of cancer-related fatigue and the associated literature supporting their effectiveness.
Introduction
Fatigue is among the most common complaints associated with cancer.[1] It can occur during or after treatment, during long-term survivorship, and in patients with extensive disease. Several instruments have been validated for use in identifying cancer-related fatigue in clinical research, such as the Brief Fatigue Inventory[2] or the Functional Assessment of Chronic Illness Therapy–Fatigue, also referred to as FACIT-F.[3] These tools, while useful, are often too unwieldly to be applied in daily practice. Instead, we usually ask “Are you bothered by fatigue?” and then attempt to classify the severity of the fatigue on a 0–10 numeric rating scale. In one study, a single-question instrument (a 0 to 10 FACES scale to score patients’ responses to the statement, “I lack energy”) had only a 3% chance of misdiagnosis.[4]
The Case
A 53-year-old previously healthy woman underwent breast cancer surgery, adjuvant combination chemotherapy with doxorubicin and cyclophosphamide, and 12 weekly cycles of paclitaxel followed by 6 weeks of radiation. She presents 3 months later with grade II peripheral neuropathy, poor sleep, and generalized fatigue. How should this patient’s fatigue be assessed and treated?
Make Sure That the Diagnosis Is Correct
Cancer-related fatigue is often multifactorial. A thorough assessment will aid in identifying the unique physiologic and psychologic factors contributing to your patients’ fatigue, allowing you to target your interventions appropriately.
Rule out medical illness. Make sure that the patient does not have treatable anemia; obstructive sleep apnea or other types of sleep disorder; poor nutrition; hypothyroidism; hypogonadism from the cancer, its treatment, or the chronic use of opioids; or a new hypopituitary state due to immunotherapy (see Table).
Evaluate the patient for depression, a confounding factor in the evaluation for fatigue. Depression is common among cancer patients; it has an overall prevalence of 21%, with depression or adjustment disorder seen in 32% of patients, and any mood disorder in 38%.[5] For our palliative oncology patients, we start with a simple question-“Are you depressed?”-which in one landmark study of 197 patients had 100% predictive value for an eventual diagnosis of depression.[6] For adult patients with cancer, the two-item Patient Health Questionnaire (PHQ-2) has a sensitivity of at least 80% and a specificity of 90%. The PHQ-2 asks the questions, “During the last month, have you often been bothered by feeling down, depressed, or hopeless?” and “During the last month, have you often been bothered by having little interest or pleasure in doing things?” Depressed cancer patients have been shown to respond well to antidepressant treatment, with an effect size of 1.56 (a 56% chance of improvement over placebo) and no worse side effects compared with placebo.[7]
Demoralization is a relatively new clinical entity with which many healthcare providers and patients are not familiar. It is part of the depressive syndromes, but has fundamentally different causes and is rooted in existential distress.[8] It can complicate fatigue or be mistaken for physical fatigue. A good working definition of demoralization is a sense of helplessness and hopelessness[9]; a feeling that the cause of distress lies outside the person (ie, is due to the disease); no anhedonia or loss of taking pleasure in previously pleasurable events (unlike patients with depression); and having some level of motivation but not knowing what actions to take.[10] In our own practice, people describe it as “sick of being so sick with no hope of that getting better,” and are often relieved that their illness has a name. They may seem listless and depressed, but their mood brightens when talking about their grandchildren or pets. It is important to listen to patients’ stories and help them by refocusing on personal coping strategies that have worked in the past[11]; we also recommend getting chaplains and social workers involved to help patients find meaning in their lives through an individualized program of dignity therapy.[12]
Nonpharmacologic Interventions
Exercise helps to alleviate fatigue, but getting patients to increase their levels of physical activity may require some one-on-one coaching from the oncology care team. Typical patient responses to exercise recommendations run along the lines of, “Doctor, I am telling you I can barely drag myself around and you are telling me I need to take a 20-minute walk twice a day?” A recent comprehensive meta-analysis showed that exercise and psychologic interventions may be the only means of alleviating cancer-related fatigue, apart from pharmacologic measures.[13] The “weighted effect size” (WES) for all exercise interventions was 0.3 (95% CI, 0.25–0.36; P < .001), or a 0.33 change in fatigue as measured on a 0–10 scale. Psychologic interventions yielded a WES of 0.27, compared with a WES of only 0.09 for pharmacologic interventions.
In considering what exercises should be recommended to patients, it is worth bearing in mind that any level of exercise seems to be of benefit. In our practice, we have found it useful to ask patients, “What types of exercises have you engaged in successfully in the past?” We encourage our patients to try yoga, cycling, swimming, and even simple walking for 10 to 20 minutes twice daily. Although supervised exercise programs have been demonstrated to be superior to self-directed interventions in decreasing fatigue, partially supervised or self-directed exercise is also known to improve fatigue compared with no exercise at all.[14-17] Patients can be supported with simple coaching, and those in need of more “hands-on” help (patients with bone metastases, thrombocytopenia, active infection, history of falls, or other potential limitations) can be referred to physical therapy or rehabilitation. As demonstrated in a recent randomized controlled trial, patients reporting the worst fatigue-likely the ones who feel they are least able to participate in physical activity-may, in fact, experience the greatest improvement in symptoms.[18]
Insomnia and sleep disturbance are prevalent in individuals facing a cancer diagnosis and can persist long after treatment ends. According to a recent systematic review of the literature, cognitive behavioral therapy for insomnia (CBT-I) should be considered first-line therapy for patients with cancer who have trouble sleeping.[18] It is more effective than pharmacologic interventions and enables patients to avoid unwanted side effects.[19] Notably, CBT-I has been shown to be beneficial in reducing fatigue in cancer patients and survivors.[20]
How can patients learn CBT-I strategies? One novel CBT-I approach available online is Sleep Healthy Using the Internet, also known as SHUTi, which was associated with a success level equivalent to that of face-to-face CBT-I.[21,22] An added bonus of SHUTi is that this program will likely improve depressive symptoms in your patients.[23] As an alternative to SHUTi, patients can be referred to a specialist who is board-certified in behavior sleep medicine and is trained to provide CBT-I.
Mindfulness-based stress reduction is an effective tool for reducing cancer-related fatigue.[24,25] It helps patients cultivate awareness and effectively cope with a variety of symptoms, including stress and pain. Many integrative medicine programs affiliated with universities offer classes in mindfulness-based stress reduction. Guided mindful practices are available in book and audio format from the founder of this practice, Jon Kabat-Zinn, PhD.
Additional complementary and alternative medicine interventions that warrant discussion include acupuncture and tai chi or qigong[26]; tai chi, across several practiced forms, focuses on meditation; breathing; and low-intensity, low-impact movement. A recent meta-analysis of randomized controlled trials found that tai chi had positive effects on cancer-related fatigue, sleep, and depression.[27,28] Acupuncture has similarly been demonstrated to be effective in improving fatigue and nausea, and may be considered as adjunctive therapy.[29] Energy conservation and activity management can improve fatigue. Arrange to have your patient meet with an occupational therapist to create an individualized plan for modifying activities of daily living.
Pharmacologic Interventions
The use of pharmacologic agents for the management of cancer-related fatigue is an evolving area of practice and study. Any recommendations to start a medication to treat cancer-related fatigue should be balanced against the available evidence to support its benefit, along with consideration of the potential adverse effects and risks associated with its use.
Steroids
Steroids are one of the most common medications used to treat fatigue and a number of other symptoms in patients receiving palliative care. Conclusions regarding their usefulness in cancer- or treatment-related fatigue are mixed, and the existing data are derived from studies focused primarily on cancer patients with advanced disease managed in a palliative care setting. A 1985 randomized clinical trial found a significant improvement in “activity” in 77% of patients receiving methylprednisolone at a dosage of 32 mg daily compared with 68% of those receiving placebo.[30] Another showed significant improvement in quality of life but did not provide specific details about the impact of this agent on fatigue as a component of the quality-of-life score.[31] Two more recent studies of 32-mg/day methylprednisolone orally for 7 days yielded conflicting results, with one demonstrating significant improvements in fatigue with treatment and the other reporting no difference from placebo.[32,33]
Dexamethasone administered at 4 mg twice a day significantly alleviated fatigue for 2 weeks in patients with advanced cancer, and was not associated with more adverse side effects than placebo.[34] While dexamethasone is our treatment of choice in this setting, we do try to prescribe the lowest dose for the shortest duration due to the lack of long-term efficacy data. In addition, adverse effects of their long-term use need to be considered; these include, but are not limited to, increased risk for thrush, edema, hyperglycemia, gastritis, and muscle weakness. Some of these conditions, in turn, may even contribute to worsening fatigue, as demonstrated in recent case reports.[35]
Stimulants
Psychostimulants are one of the most widely studied pharmaceutical classes used for the treatment of cancer-related fatigue. This drug class includes methylphenidate, D-methylphenidate, dextroamphetamine, modafinil, and armodafinil. Most randomized controlled trials have been conducted with methylphenidate and modafinil; however, the results have been mixed, with several studies showing no benefit. Secondary analyses have shown that patients with more severe fatigue or more advanced disease may benefit from the use of psychostimulants, whereas those with mild to moderate fatigue do not.[36,37] Day 1 responses predict longer-duration responses with 85% accuracy, so the drug can be stopped in a few days if it is found to be ineffective.[38] In practice, we find that patients who benefit the most from these agents are those with fatigue scores of 8 to 10 out of 10. We give these patients a 5-day trial of methylphenidate at a dose of 5 mg; if no benefit is seen, then the treatment is stopped.
Other agents
Two studies have evaluated the selective serotonin reuptake inhibitor paroxetine for fatigue and have not found any benefits from treatment.[39,40] Studies of the acetylcholinesterase inhibitor donepezil[41] to alleviate cancer-related fatigue and of testosterone in fatigued men with cancer and low testosterone levels[42] have also not shown any significant differences compared with placebo.
American ginseng (Panax quinquefolius) was evaluated in a dose-finding randomized controlled trial in which it was administered at a dose of 750 to 2,000 mg daily for 8 weeks.[43] Although no significant difference in fatigue was found between groups, there was a trend to effect among patients who received ginseng at higher doses. As a result, the investigators conducted a second study in which 364 patients received the 2,000-mg daily dose; they identified a significant improvement in physical fatigue at 8 weeks.[44] High-dose Asian ginseng (Panax ginseng) appeared to be promising in a phase II trial, but in a small randomized trial it was found to be no better than placebo.[45]
Likewise, extract from the highly caffeinated guarana (Paullinia cupana) plant at a dosage of 50 mg orally twice daily[46] and extract from bojungikki-tang (a mixture of 10 medicinal plants) at a dosage of 2.5 g thrice daily[47] have been shown to statistically significantly reduce fatigue after 3 weeks and 2 weeks of treatment, respectively.[46,47]
Studies of melatonin (also known as N-acetyl-5-methoxytryptamine) administered at a 20-mg dose orally for 1 week[48] and L-carnitine (a naturally occurring dipeptide comprising the essential amino acids lysine and methionine) given at a dosage of 2 g per day[49] showed no benefit in patients with fatigue. However, a recent Japanese study of a proprietary amino acid jelly containing coenzyme Q10 and L-carnitine did show an improvement in fatigue in breast cancer patients receiving chemotherapy.[50]
Summary
Cancer-related fatigue is a common, albeit complex, symptom experienced by many cancer patients. Identification of fatigue and assessment of its severity should be a part of routine office care and can be performed using simple, one-question screening tools. It is important to identify physiologic and psychologic factors contributing to your patient’s fatigue, if possible, and target interventions for any treatable causes (anemia, hypothyroidism, depression, etc). Encourage nonpharmacologic interventions like exercise as first-line treatment, and reserve pharmacologic approaches for patients in whom the modest expected improvements outweigh potential adverse effects.
Financial Disclosure: Dr. Smith has received travel funding for teaching from GEOMC Co, Ltd. The other authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Berger AM, Mooney K, Alvarez-Perez A, et al. Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw. 2015;13:1012-39.
2. Mendoza TR, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186-96.
3. FACIT.org. Questionnaires. http://www.facit.org/FACITOrg/Questionnaires. Accessed September 28, 2017.
4. Baussard L, Stoebner-Delbarre A, Bonnabel L, et al. Development and validation of the daily fatigue cancer scale (DFCS): single-item questions for clinical practice. Eur J Oncol Nurs. 2017;26:42-8.
5. Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160-74.
6. Chochinov HM, Wilson KG, Enns M, Lander S. “Are you depressed?” Screening for depression in the terminally ill. Am J Psychiatry. 1997;154:674-6.
7. Laoutidis ZG, Mathiak K. Antidepressants in the treatment of depression/depressive symptoms in cancer patients: a systematic review and meta-analysis. BMC Psychiatry. 2013;13:140.
8. Grassi L, Nanni MG. Demoralization syndrome: new insights in psychosocial cancer care. Cancer. 2016;122:2130-3.
9. Robinson S, Kissane DW, Brooker J, Burney S. A review of the construct of demoralization: history, definitions, and future directions for palliative care. Am J Hosp Palliat Care. 2016;33:93-101.
10. Caruso R, GiuliaNanni M, Riba MB, et al. Depressive spectrum disorders in cancer: diagnostic issues and intervention. A critical review. Curr Psychiatry Rep. 2017;19:33.
11. Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36:733-42.
12. Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12:753-62.
13. Mustian KM, Alfano CM, Heckler C, et al. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA Oncol. 2017;3:961-8.
14. Velthuis MJ, Agasi-Idenburg SC, Aufdemkampe G, Wittink HM. The effect of physical exercise on cancer-related fatigue during cancer treatment: a meta-analysis of randomised controlled trials. Clin Oncol (R Coll Radiol). 2010;22:208-21.
15. Shelton ML, Lee JQ, Morris GS, et al. A randomized controlled trial of a supervised versus a self-directed exercise program for allogeneic stem cell transplant patients. Psychooncology. 2009;18:353-9.
16. Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients-a systematic review of randomized controlled trials. Support Care Cancer. 2012;20:221-33.
17. Schuler MK, Hentschel L, Kisel W, et al. Impact of different exercise programs on severe fatigue in patients undergoing anticancer treatment-a randomized controlled trial. J Pain Symptom Manage. 2017;53:57-66.
18. Garland SN, Johnson JA, Savard J, et al. Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsych Dis Treat. 2014;10:1113-24.
19. Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch Intern Med. 2004;164:1888-96.
20. Fleming L, Randell K, Harvey C, Espie CA. Does cognitive behaviour therapy for insomnia reduce clinical levels of fatigue, anxiety and depression in cancer patients? Psychooncology. 2014;23:679-84.
21. Ritterband LM, Thorndike FP, Ingersoll KS, et al. Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: a randomized clinical trial. JAMA Psychiatry. 2017;74:68-75.
22. Seyffert M, Lagisetty P, Landgraf J, et al. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PloS One. 2016;11:e0149139.
23. Christensen H, Batterham PJ, Gosling JA, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight study): a randomised controlled trial. Lancet Psychiatry. 2016;3:333-41.
24. Johns SA, Brown LF, Beck-Coon K, et al. Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psychooncology. 2015;24:885-93.
25. Reich RR, Lengacher CA, Alinat CB, et al. Mindfulness-based stress reduction in post-treatment breast cancer patients: immediate and sustained effects across multiple symptom clusters. J Pain Symptom Manage. 2017;53:85-95.
26. Klein P, Schneider R, Rhoads C. Qigong in cancer care: a systematic review and construct analysis of effective qigong therapy. Support Care Cancer. 2016;24:3209-22.
27. Xiang Y, Lu L, Chen X, Wen Z. Does tai chi relieve fatigue? A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2017;12:e0174872.
28. Zhang LL, Wang SZ, Chen HL, Yuan AZ. Tai chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage. 2016;51:504-11.
29. Wu X, Chung VC, Hui EP, et al. Effectiveness of acupuncture and related therapies for palliative care of cancer: overview of systematic reviews. Sci Rep. 2015;5:16776.
30. Bruera E, Roca E, Cedaro L, et al. Action of oral methylprednisolone in terminal cancer patients: a prospective randomized double-blind study. Cancer Treat Rep. 1985;69:751-4.
31. Della Cuna GR, Pellegrini A, Piazzi M. Effect of methylprednisolone sodium succinate on quality of life in preterminal cancer patients: a placebo-controlled, multicenter study. The Methylprednisolone Preterminal Cancer Study Group. Eur J Cancer Clin Oncol. 1989;25:1817-21.
32. Eguchi K, Honda M, Kataoka T, et al. Efficacy of corticosteroids for cancer-related fatigue: a pilot randomized placebo-controlled trial of advanced cancer patients. Palliat Support Care. 2015;13:1301-8.
33. Paulsen Ã, Klepstad P, Rosland JH, et al. Efficacy of methylprednisolone on pain, fatigue, and appetite loss in patients with advanced cancer using opioids: a randomized, placebo-controlled, double-blind trial. J Clin Oncol. 2014;32:3221-8.
34. Yennurajalingam S, Frisbee-Hume S, Palmer JL, et al. Reduction of cancer-related fatigue with dexamethasone: a double-blind, randomized, placebo-controlled trial in patients with advanced cancer. J Clin Oncol. 2013;31:3076-82.
35. Matsuo N, Yomiya K. Aggravation of fatigue by steroid therapy in terminally ill patients with cancer. Am J Hospice Palliat Med. 2014;31:341-4.
36. Jean-Pierre P, Morrow GR, Roscoe JA, et al. A phase 3 randomized, placebo-controlled, double-blind, clinical trial of the effect of modafinil on cancer-related fatigue among 631 patients receiving chemotherapy. Cancer. 2010;116:3513-20.
37. Moraska AR, Sood A, Dakhil SR, et al. Phase III, randomized, double-blind, placebo-controlled study of long-acting methylphenidate for cancer-related fatigue: North Central Cancer Treatment Group NCCTG-N05C7 trial. J Clin Oncol. 2010;28:3673-9.
38. Yennurajalingam S, Palmer JL, Chacko R, Bruera E. Factors associated with response to methylphenidate in advanced cancer patients. Oncologist. 2011;16:246-53.
39. Morrow GR, Hickok JT, Roscoe JA, et al. Differential effects of paroxetine on fatigue and depression: a randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol. 2003;21:4635-41.
40. Roscoe JA, Morrow GR, Hickok JT, et al. Effect of paroxetine hydrochloride (Paxil) on fatigue and depression in breast cancer patients receiving chemotherapy. Breast Cancer Res Treat. 2005;89:243-9.
41. Bruera E, El Osta B, Valero V, et al. Donepezil for cancer fatigue: a double-blind, randomized, placebo-controlled trial. J Clin Oncol. 2007;25:3475-81.
42. Del Fabbro E, Garcia JM, Dev R, et al. Testosterone replacement for fatigue in hypogonadal ambulatory males with advanced cancer: a preliminary double-blind placebo-controlled trial. Support Care Cancer. 2013;21:2599-607.
43. Barton DL, Soori GS, Bauer BA, et al. Pilot study of Panax quinquefolius (American ginseng) to improve cancer-related fatigue: a randomized, double-blind, dose-finding evaluation: NCCTG trial N03CA. Support Care Cancer. 2010;18:179-87.
44. Barton DL, Liu H, Dakhil SR, et al. Wisconsin ginseng (Panax quinquefolius) to improve cancer-related fatigue: a randomized, double-blind trial, N07C2. J Natl Cancer Inst. 2013;105:1230-8.
45. Yennu S, Tannir NM, Williams JL, et al. Effects of high-dose Asian ginseng (Panax ginseng) to improve cancer-related fatigue: results of a double-blind, placebo-controlled randomized controlled trial. J Clin Oncol. 2016;34(26 suppl):abstr 209.
46. de Oliveira Campos MP, Riechelmann R, Martins LC, et al. Guarana (Paullinia cupana) improves fatigue in breast cancer patients undergoing systemic chemotherapy. J Altern Complement Med. 2011;17:505-12.
47. Jong Soo Jeong JS, Bong Ha Ryu BH, Jin Sung Kim JS, et al. Bojungikki-tang for cancer-related fatigue: a pilot randomized clinical trial. Integr Cancer Ther. 2010;9:331-8.
48. Lund Rasmussen C, Klee Olsen M, Thit Johnsen A, et al. Effects of melatonin on physical fatigue and other symptoms in patients with advanced cancer receiving palliative care: a double-blind placebo-controlled crossover trial. Cancer. 2015;121:3727-36.
49. Cruciani RA, Zhang JJ, Manola J, et al. L-carnitine supplementation for the management of fatigue in patients with cancer: an Eastern Cooperative Oncology Group phase III, randomized, double-blind, placebo-controlled trial. J Clin Oncol. 2012;30:3864-9.
50. Iwase S, Kawaguchi T, Yotsumoto D, et al. Efficacy and safety of an amino acid jelly containing coenzyme Q10 and L-carnitine in controlling fatigue in breast cancer patients receiving chemotherapy: a multi-institutional, randomized, exploratory trial (JORTC-CAM01). Support Care Cancer. 2016;24:637-46.