Sunitinib Still Standard First-Line Treatment for Metastatic RCC
Results of a head-to-head comparison of first-line treatment of metastatic renal cell carcinoma with the mTOR inhibitor everolimus or VEGF inhibitor sunitinib showed that everolimus did not meet noninferiority requirements as a first-line therapy.
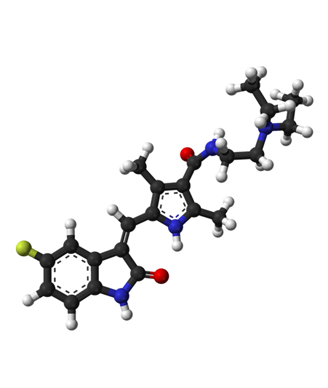
Ball-and-stick model of sunitinib.
Results of a head-to-head comparison of first-line treatment of metastatic renal cell carcinoma with the mTOR inhibitor everolimus or VEGF inhibitor sunitinib showed that everolimus did not meet noninferiority requirements as a first-line therapy. Instead, results of the RECORD-3 trial supported the continued use of sunitinib as first-line therapy in these patients.
“The observed median progression-free survival was shorter for first-line everolimus than for first-line sunitinib,” wrote Robert J. Motzer, MD, of Memorial Sloan Kettering Cancer Center, and colleagues in the Journal of Clinical Oncology. “These clinically relevant differences support the standard treatment sequence, whereby patients who experience progression on (or are intolerant of) first-line sunitinib are subsequently treated with everolimus.”
Results of RECORD-3 were initially presented at the 2013 ASCO Annual Meeting.
RECORD-3 was a phase II crossover trial designed to evaluate first-line everolimus followed by sunitinib at progression compared with first-line sunitinib followed by everolimus at progression. According to the researchers, the hypothesis for the design of this study was that “similar combined progression-free survival lengths would be achieved by both sequences and that everolimus would be better tolerated than sunitinib as the ï¬rst-line therapy.”
The trial included 471 patients who were randomly assigned to first-line everolimus (n = 238) or sunitinib (n = 233); 108 patients eventually crossed over from everolimus to sunitinib and 99 crossed over from sunitinib to everolimus.
The median progression-free survival of patients assigned first-line everolimus was 7.9 months compared with 10.7 months for patients assigned first-line sunitinib (HR = 1.4; 95% CI, 1.2-1.8). The combined progression-free survival was both regimens was 25.8 months for sequential sunitinib then everolimus compared with 21.1 months for sequential everolimus then sunitinib. The median overall survival for first-line everolimus was 22.4 months compared with 32 months for first-line sunitinib (HR = 1.2; 95% CI, 0.9-1.6).
A prespecified analysis looked at the efficacy of the two drugs across a series of patient subgroups. Median progression-free survival was longer for patients with intermediate- and favorable-risk disease treated with first-line sunitinib compared with everolimus. In addition, those patients with clear cell and non-clear cell histology also had longer progression-free survival with sunitinib.
“The observed adverse events were consistent with the known safety profiles of everolimus and sunitinib and differentiated by their respective mTOR inhibitor and VEGFR tyrosine kinase inhibitor class,” the researchers wrote.
RECORD-3 was sponsored by Novartis Pharmaceuticals.