Surgery in the Older Patient
Surgery is still the most important treatment for solid tumors, regardless of the age of the patient. In this article, we discuss the physiology of aging as it relates to risk assessment in the elderly surgical oncology patient. A brief review of the role of surgery in the treatment of breast, colorectal, pancreatic, and gastric cancer is provided, because these solid tumors primarily affect elderly patients.
ABSTRACT: Surgery is still the most important treatment for solid tumors, regardless of the age of the patient. In this article, we discuss the physiology of aging as it relates to risk assessment in the elderly surgical oncology patient. A brief review of the role of surgery in the treatment of breast, colorectal, pancreatic, and gastric cancer is provided, because these solid tumors primarily affect elderly patients. Options for palliation are discussed. We conclude that older patients should not be deprived of curative surgery based on chronologic age alone. [ONCOLOGY 16:183-199, 2002]
The population of the United States is growing and aging. Because the incidence of cancer, particularly solid tumors, increases with age, the number of elderly patients with cancer who require surgical intervention is expected to rise markedly in the next decade. Surgery remains the most important treatment for solid tumors, regardless of the patient’s age. In hematologic malignancies such as lymphoma and leukemia, surgery is often required for diagnosis and consolidation of treatment. The most common tumors in elderly patients-colorectal, breast, gastric, and pancreatic cancer-require surgery for cure.
Because clinicians often underestimate the life expectancy of elderly patients, cancer in these patients is frequently undertreated. Inadequate initial therapy for an older cancer patient can result in recurrence, metastasis, or death. Not only are these outcomes potentially preventable with appropriate intervention, they can also have a severe impact on the quality of life of the elderly patient, in whom preservation of quality of life is paramount.
Choosing Therapy for the Elderly
The elderly tend to be underrepresented in most clinical trials, and as a result, optimal therapy for elderly cancer patients is not always clearly delineated. This is particularly true of trials with a surgical component. Scientific data from randomized studies are not available for the older population, and most available information comes from retrospective studies.
According to the Metropolitan Life Insurance tables, life expectancy in the United States continues to rise. Thus, it is likely that the grass roots efforts of groups interested in the health and welfare of the elderly will demand and receive appropriate inclusion in federally funded clinical studies. Until that time, the limited information available on outcomes in elderly cancer patients will have to be used along with the judgment of clinicians who treat and operate on elderly patients to determine the appropriate therapy for an individual.
Many factors influence the selection of therapy for elderly patients. There is growing interest in trying to establish physiologic age as opposed to relying solely on chronologic age as a means of determining whether a patient may be a candidate for surgery. Comorbid diseases, decreased functional status, limited economic resources, and cognitive status clearly affect outcome in elderly cancer patients. However, clinician biases such as perceived limited life expectancy due to chronologic age and assumed fragility and inability to tolerate treatment may be preventing elderly cancer patients from receiving the appropriate definitive therapy for a specific malignancy.
Quality of life is often the most important factor when deciding on whether to pursue curative or palliative options for a cancer diagnosis in elderly patients. Because surgery, by its nature, diminishes the quality of life of all patients regardless of age in the short term (with the expectation of improving or extending quality of life in the long term), it is often shunned by both patients and referring physicians. For the elderly patient considering surgical management, the risk of diminishing quality of life in the long term may be considered prohibitive.
However, current literature does not support this perception. Although cancer procedures are often complex and carry with them significant morbidity and mortality, appropriate and accurate counseling of patients and their supporters can minimize fear and produce realistic expectations. This article reviews the current knowledge regarding risk assessment and surgical management of some of the most common solid tumors found in the elderly.
Risk Assessment
Risk assessment in the elderly involves the interaction of the underlying physiologic status-including the normal physiologic changes of aging and those attributed to comorbid disease-the disease process, the surgical procedure, and the type of anesthesia required for the operation. Chronologic age alone should not be the sole criterion for assessing surgical risk in the elderly cancer patient. Attempts have recently been made to calculate physiologic age as a predictor of outcome.
In one study of more than 250 patients aged 70 years or older who underwent elective abdominal surgery under general anesthesia, 24 preoperative variables were compared between patients who left the hospital in satisfactory condition and those who died in the hospital despite the operative procedure performed.[1] Although no significant differences were found in the group aged 70 to 79 years, there was a significant difference in performance status and total lymphocyte count in the group over age 80 years. When combined with age, a computer-generated discriminant function analysis yielded an equation that calculated survival with 97% accuracy and mortality with 83% accuracy. This crude method of determining outcome was an attempt to combine chronologic age with variables that reflect the normal physiologic changes that occur with aging.
Cardiovascular Complications
Every major organ system undergoes changes in its physiology with age, and this can affect response to surgery.[2] Cardiovascular complications are commonly associated with major surgery in the elderly. Atherosclerotic disease, dysrhythmias, and conduction disturbances are more common with age. Volume depletion is not well tolerated in the elderly, because the aged body relies more on preload to increase cardiac output, due to a generalized decrease in the distensibility of the cardiac wall. Complex cancer operations often involve significant fluid shifts that may cause more morbidity in elderly patients.
TABLE 1
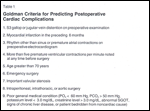
Goldman Criteria for Predicting Postoperative Cardiac Complications
The Goldman criteria were developed by multivariate analysis to predict cardiac complications independently in patients undergoing noncardiac surgery (Table 1).[3] By ranking these factors, a patient can be assigned to one of four risk categories that correlate well with the risk for cardiac death. Chronologic age is one factor, but the type and nature of the surgery as well as the clinical evaluation of the patient’s cardiac status contribute more significantly to the patient’s ranking.
Hepatic and Psychological Changes
Liver function also changes with age because of decreased liver mass, blood flow, and perfusion.[4] Histologic and metabolic changes that decrease the ability of the liver to metabolize drugs occur with age and result in an increase in the half-life of many drugs. Furthermore, the need for multiple medications, common in the elderly, is known to increase the risk of adverse drug reactions caused by hepatic dysfunction.
Dementia and depression commonly develop in the postoperative period among the elderly. Reductions in the number of neurons, cerebral blood flow, metabolic oxygen consumption, and number of receptor sites for neurotransmitters contribute to an increased sensitivity to drugs in the elderly and can lead to postoperative delirium.[5] Anesthetic agents and postoperative analgesics must be used with caution to avoid postoperative changes in mental status, delirium, hypoventilation, and anoxia.
Surgical Risk Assessment
TABLE 2
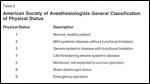
American Society of Anesthesiologists General Classification of Physical Status
Surgical risk can be assessed in several ways. One of the most widely used tools for estimating risk from anesthesia alone is the American Society of Anesthesiologists (ASA) General Classification of Physical Status. The mortality rate, as related to anesthesia, is classified in one of five categories depending on the physical status of the patient (Table 2).[6]
Increases in morbidity and mortality are generally associated with emergency surgery and advanced disease states.[7-9] Because many elderly patients present with advanced disease (often because of a delay in diagnosis), they tend to require more emergency interventions that ultimately increase their surgical risk. Appropriate screening, earlier diagnosis, and earlier surgery can diminish the risk of surgery in elderly cancer patients.
Breast Cancer
Breast cancer is the most common cancer in women in the United States. In 2001, an estimated 192,200 new cases of female breast cancer were diagnosed.[10] The incidence of breast cancer rises with age, with more than 40% of breast cancers developing in women aged 70 years or older.[11] Because life expectancy continues to rise in Western countries with a high incidence of breast cancer, an appropriate treatment regimen for elderly breast cancer patients needs to be determined.
Breast cancer occurs in the elderly in much the same way as in younger patients. The majority of patients present with stage I or II disease and are generally considered candidates for surgery.[12] However, the elderly tend to present with more hormone receptor-positive tumors- usually a favorable sign.[12]
There is still much debate about what treatment should be offered to the elderly breast cancer patient, because the elderly have largely been excluded from clinical trials that have determined therapy in other age groups. Prospective trials have recently been initiated to help settle the debates, but it will take several years for the data to mature. A larger review of this topic will be covered in this series in a subsequent issue. Nevertheless, since surgery is the mainstay of treatment for breast cancer, a brief review of the current literature focusing on surgical management is in order.
Studies in Older Patients
At least one study suggests that elderly breast cancer patients may be undertreated by acceptable standards.[13] In this review of 351 patients more than 65 years old from the Rhode Island tumor registry, 26% of stage I patients were treated with lumpectomy alone, instead of the usual treatment of lumpectomy followed by radiation therapy. The 5-year survival of this group was significantly worse than that of patients treated either by mastectomy or lumpectomy with axillary node dissection and radiotherapy.
Recently, there has been interest in using tamoxifen (Nolvadex) as an adjuvant therapy to prevent recurrence of disease in patients who have undergone limited surgical excision for breast cancer. Several retrospective and small prospective series suggest that this may, in fact, be an appropriate option for elderly patients who wish to undergo breast conservation therapy but who do not wish or are not candidates for radiation therapy.[12,14] Larger prospective randomized trials are currently under way to determine whether lumpectomy (without axillary node clearance and/or radiation) and tamoxifen is an acceptable alternative for elderly patients with early breast cancer.
It is rare that a patient is unable to undergo surgery for breast cancer. The most aggressive surgical management, the modified radical mastectomy, is well tolerated by all but the most debilitated of patients. In an institutional review by Termuhlen (unpublished data), 24 of 29 patients aged 80 years or older with newly diagnosed breast cancer underwent surgical therapy as a key component in the management of their breast cancer. There were no deaths. The most serious complication was a wound hematoma in one patient who required repeat surgery and ultimately recovered without further sequelae. The patients ranged in age from 80 to 106 years. The oldest patient was 106 years and 10 months at the time of her second mastectomy, the first having been performed at age 96 years for a contralateral breast cancer.
Similar results have been noted in centenarians. A study in 31 patients aged 100 to 107 years treated at Mayo Clinic-affiliated hospitals showed only a 3% complication rate and no mortality associated with surgical interventions (including breast procedures) under anesthesia.[15]
• Conclusions-Appropriate initial management of breast cancer in the elderly can prevent the debilitating effects of metastatic disease and locoregional recurrences. The majority of patients are able to tolerate surgical procedures for diagnosis and treatment of breast cancer even in the presence of significant comorbid conditions. Breast conservation therapy with limited axillary dissections and the use of tamoxifen may become the standard of care for the elderly patient. Completion of prospective randomized studies directed at determining the options for breast cancer management in elderly patients are anxiously awaited.
Colorectal Cancer
Colorectal cancer is the second most common cause of cancer death in the United States. Over 135,000 cases were diagnosed in 2001.[10] Because half of all colorectal cancer patients are diagnosed at age 65 years or older, the number of colorectal cancer cases will rise as the population ages.
Surgical resection of the colon or rectum remains the mainstay of curative treatment for colorectal cancer. Even if metastatic disease is present at the time of diagnosis, resection of the primary lesion is often necessary. Bleeding, obstruction, and perforation can occur if the primary tumor is not attended to. Several retrospective studies have examined the risk of surgical resection in the elderly. Morbidity and mortality is higher in this population, perhaps as a result of the increased incidence of emergency surgery among these patients. Studies have shown that patients more than 70 years old present with more advanced disease and have an increased incidence of palliative and definitive surgical procedures performed on an emergency basis, contributing to the higher rates of morbidity and mortality.[16-18]
Nevertheless, given the same type of surgery (ie, emergent or elective), when results in elderly patients are compared with those in control subjects, patients of advanced age retain an increased risk of postoperative complications. These differences are related to the overall physiologic condition of the patient as opposed to the chronologic age. Cardiovascular disease, pulmonary dysfunction, and advanced American Society of Anesthesiology (ASA) score have all been found to increase postoperative morbidity and mortality, independent of chronologic age.[19-22]
Postoperative Complications and Survival
Cardiopulmonary complications are the most common cause of postoperative morbidity and mortality. In one series, cardiopulmonary complications ranged from 1.8% in patients under age 65 years to 10.8% in patients aged 65 to 75 years. Patients more than 75 years old had a complication rate of 8.2%.[21] The rate of anastomotic leak in elderly patients as compared to younger patients is controversial. Some studies have reported an increased rate, whereas others report no difference.[21,22]
TABLE 3

Mortality Rates for Elderly Patients Undergoing Colorectal Surgery
In the majority of elderly patients who die in the postoperative period after colorectal surgical procedures, death is generally caused by systemic (primarily cardiopulmonary) complications. In younger patients, anastomotic leak is the most common cause of mortality.[21] Mortality rates for colorectal surgery in elderly patients range from 1.3% to 8.2% for elective procedures to more than 20% for emergency cases (Table 3).[21,23-28] Older literature suggests that there is an increased incidence of mortality among elderly patients who undergo colorectal surgery; recent literature does not support this correlation.[26-28] Postoperative mortality is more a function of the physiologic state of the patient than the patient’s chronologic age.
In one study, survival after curative resection was reported to be lower for patients more than 70 years old.[29] However, in another series, multivariate analysis demonstrated that the 3-year survival rate is influenced by disease stage and type of surgery performed (curative vs palliative), and not by an age older or younger than 80 years.[30] This is supported by another study in which the disease-specific survival rate was not significantly different in patients 75 years of age or older vs younger patients, with a median follow-up of 48 months.[28] Additional studies have supported the finding that 5-year survival rates for older patients are equivalent to those of younger patients if curative resection is performed in patients who are appropriate candidates for surgery.[31]
Hepatic Resection
The current recommendation for patients with limited metastatic disease from colorectal cancer-usually less than three lesions confined to the liver-is to undergo hepatic resection. Long-term survival following hepatic resection for colorectal metastases is not clearly influenced by age. No significant difference in median survival was found in two studies that compared survival in patients older and younger than 60 or 70 years, respectively.[32,33] However, elderly patients appear to have a decreased tolerance for extended resections because of limited functional reserve and lower regenerative capability.
In one series, 60% of all deaths after hepatic resection in patients aged 65 to 82 years was attributed to hepatic failure. Most of these patients had undergone extended resections such as right trisegmentectomies.[34] Thus, while elderly patients may receive the same survival benefit as younger patients who are candidates for hepatic resection of colorectal metastases, careful selection of patients is urged with an emphasis on the volume of liver resected.
Pancreatic Cancer
More than two-thirds of patients diagnosed with pancreatic cancer are more than 65 years old at the time of diagnosis,[35] and most present with metastatic disease precluding the possibility of undergoing pancreatic resection for cure. The few candidates for surgical resection most commonly undergo pancreaticoduodenectomy. In most recent large series, this procedure is associated with complication and mortality rates of less than 5%.[36] Several recent studies have examined the safety and efficacy of pancreatic resection in the elderly.
Studies in Older Patients
One series focused on the safety of pancreaticoduodenectomy in patients aged 70 years or older. Postoperative mortality and morbidity and long-term survival rates of 74 consecutive patients who underwent subtotal pancreatic resection for cancer in the periampullary region were compared to those of a younger group of patients.[37] The groups were matched for sex, preoperative weight loss, extent of surgery, tumor size and grade, and presence of lymph node metastases. There was no difference in estimated blood loss, operative time, and length of hospital stay.
Complication and mortality rates were equivalent. Perioperative mortality for the elderly patients was 7%, compared with 4% in the younger group. Long-term survival was equivalent in the two age groups when all histologic diagnoses were considered, as well as when pancreatic adenocarcinoma patients were analyzed separately. The authors concluded that chronologic age alone is not a contraindication for curative pancreatic resection.
In another series that evaluated whether age is a risk factor for major pancreatic resection, 300 patients aged 23 to 83 years were evaluated in a prospective case control study.[38] A partial or total pancreaticoduodenectomy was performed in 228 patients aged 23 to 83 years, with a mean age of 61 years. Distal pancreatectomy was performed in 72 patients aged 28 to 86 years, with a mean age of 65 years.
Complications from pancreaticoduodenectomy developed in 22.1% of patients aged 70 years or younger, and in 30.2% of patients more than 70 years old. A significant difference was noted in the systemic complications that developed in 16.1% of the younger group and 27.9% of the older group. There was no significant difference in mortality rates between the groups. Mortality rates at 30 and 90 days after surgery were 3.2% and 6% for the younger group and 2.3% and 6.9% for the older group, respectively. Regression analysis showed that preoperative serum bilirubin, diameter of the pancreatic duct, intraoperative blood loss, and the occurrence of surgical or systemic complications exert an independent influence on mortality. Age was not an independent variable in the prognosis of morbidity or mortality.
In patients who underwent a distal pancreatectomy, a significant difference was seen again in the rate of systemic complications, with a higher rate noted in the older group. No significant difference was seen in the 30- and 90-day mortality rates. Intraoperative blood loss was noted as an independent influence on morbidity and mortality; however, age had no independent influence. The authors concluded that while systemic complications developed more frequently in the older group, age was not an independent risk factor for mortality.
Higher complication rates were seen by another group that compared patients aged 80 years or older who underwent pancreaticoduodenectomy with younger patients undergoing the same procedure.[39] A slightly higher but still insignificant difference in mortality was noted in the older group (4.2% vs 1.6%), but there was no difference in 5-year survival between the two groups. The authors agreed that age alone should not be a contraindication for pancreaticoduodenectomy.
Gastric Cancer
Nearly 50% of men and 60% of women diagnosed with gastric cancer in the United States are more than 70 years old.[40] The primary treatment for gastric cancer is surgical resection, with subtotal or total gastrectomy the procedure of choice. Regardless of age, these procedures carry a significant morbidity and mortality.
Preoperative risk factors, such as cardiopulmonary disease and malnutrition, are increased in elderly patients with gastric cancer and are associated with higher complication rates following surgery.[41] Rates of surgically related complications such as anastomotic leak or intra-abdominal abscess are similar in older and younger patients.[42-44] However, systemic complications develop more commonly after gastric surgery in elderly patients, similar to findings noted in older patients who undergo pancreaticoduodenectomy.[43] Once again, the 5-year survival rate of curatively resected patients with gastric cancer was similar for younger and older patients.[45]
Palliative Surgery
While quality of life is an important consideration for patients of any age, it is often the main consideration for elderly patients. Careful patient selection with consideration of physiologic status as opposed to chronologic age is the main determinant in successful completion of curative resections in older cancer patients. When cure is not possible, surgeons are often faced with the need for palliation. This is particularly true in patients with gastrointestinal malignancies. Experienced clinicians know that palliative surgical procedures in patients of any age are often fraught with serious morbidity and high mortality rates. However, once again, careful patient selection and preparation can minimize poor outcomes and help patients maintain a reasonable quality of life.
In the preoperative period, it is important to meet the family and others who provide support to the patient. This is critical for elderly patients who have some element of mental impairment. Such individuals may need extra time and assistance to grasp the nature of the planned procedure and its risks and benefits. Establishing a health-care power of attorney and engaging these patients in the preoperative counseling can ease decision-making in the event of a poor outcome. Allowing patients to express their wishes verbally regarding cardiopulmonary resuscitation or extraordinary measures in the event of cardiopulmonary collapse gives both the surgeon and the patient’s family the opportunity to know exactly what the patient’s wishes are.
Outcome Goals
Goal-setting is extremely important when deciding which palliative procedures to pursue. The direct way to know what patients expect is to ask them. If returning to an independent lifestyle is the expectation, then providing patients and their caregivers with a realistic estimate of that likelihood is recommended. If an intermediate setting such as rehabilitation or a skilled nursing facility is anticipated, estimating the length of time in the facility can help the patient and family cope with the change.
For patients who want an extension of life until, for example, the birth of a grandchild, knowing this fact can help the clinician in deciding how aggressive to be with treatment. Ultimately, everyone benefits from a realistic discussion of the risks and benefits and chance of mortality associated with the planned procedure. Preparation on the part of both the patient and the surgeon can help achieve as many of the goals of palliation as possible.
For patients who are not surgical candidates, palliation may still be provided via minimally invasive or percutaneous methods. Obstruction of the biliary tree that often occurs with pancreatic cancer can be palliated by the use of internal stents in the bile duct. These can be placed percutaneously or preferably via endoscope. Semipermanent stents (eg, Wallstents) are often a good choice to minimize repeat procedures and avoid surgical bypass in the patient who is debilitated and has metastatic disease. Several studies have suggested that these stents maintain good quality of life in patients with unresectable malignancies.[46,47]
Patients who have advanced rectal cancer can benefit from local therapies such as fulguration, laser therapy, or cryotherapy. Laser therapy provides effective palliation of obstruction in 85% to 95% of patients with low morbidity and mortality.[48] Endoscopically placed, endoluminal expandable colonic stents can also provide excellent palliation and avoid the need for surgical intervention.[49]
Summary
Because the incidence of most cancers increases with age, it is often the elderly patient who must deal with the diagnosis and treatment of a malignancy. The risk of surgical intervention is usually a function of the physiologic state of the patient as opposed to the chronologic age. Standard therapy for a specific malignancy should be considered for the elderly cancer patient, despite the lack of inclusion of older patients in many clinical protocols that have determined the standard of care.
Attention to the normal physiologic changes associated with aging can help the surgeon to adequately prepare the elderly patient for surgery and to safely complete the planned procedure. Quality of life should be considered in all patients. An honest dialog between patients, their supporters, and the surgeon can help all parties be realistic about expectations for recovery and maintenance of quality of life after surgery for cancer.
References:
1. Masuo K, Kumagai K, Tanaka T, et al: "Physiological" age as anoutcome predictor for abdominal surgery in elderly patients. Surg Today28(10):997-1000, 1998.
2. Evers BM, Townsend CM, Thompson JC: Organ physiology of aging. Surg ClinNorth Am 74:23-39, 1994.
3. Goldman L, Caldera DC, Nussbaum SR, et al: Multifactorial index of cardiacrisk in noncardiac surgical procedures. N Engl J Med 297:845, 1977.
4. Wynne HA, Cope LH, Mutch E, et al: The effect of age upon liver volume andapparent liver blood flow in healthy man. Hepatology 9:297-301, 1989.
5. Buxbaum JL, Schwartz AJ: Perianesthetic considerations for the elderlypatient. Surg Clin North Am 74:41-58, 1994.
6. Rutter TW, Tremper KK: Anesthesiology and pain management, preoperativeevaluation, Table 13-10, in Greenfield LJ, Mulholland MW, Oldham KT, et al (eds):Surgery: Scientific Principles & Practice, 2nd ed, p 446. Philadelphia-NewYork, Lippincott-Raven, 1997.
7. Gagner M: Value of preoperative physiologic assessment in outcome ofpatients undergoing major surgical procedures. Surg Clin North Am 71:1141-1150,1991.
8. Hoskins MP, Warner MA, Lobdell CM, et al: Outcomes of surgery in patients90 years of age and older. JAMA 261:1909-1915, 1989.
9. Reiss R, Deutsch AA, Nudelman I: Abdominal surgery in elderly patients:Statistical analysis of clinical factors prognostic of mortality in 1000 cases.Mt Sinai J Med 54:135-140, 1987.
10. Greenlee RT, Hill-Harmon MB, Murray T, et al: Cancer statistics, 2001. CACancer J Clin 51(1):15-36, 2001.
11. Marbelli G, De Palo G: Breast cancer in elderly women (70 years or more):Which treatment? Tumori 85(6):421-424, 1999.
12. Busch E, Kemeny MM, Fremgen A, et al: Patterns of breast cancer in theelderly. Cancer 78:101-111, 1996.
13. Wanebo JH, Cle B, Chung M, et al: Is surgical management compromised inelderly patients with breast cancer? Ann Surg 225:579-589, 1997.
14. Gori J, Castano R, Engel H, et al: Conservative treatment vs mastectomywithout radiotherapy in aged women with breast cancer-a prospective andrandomized trial. Zentralbl Gynakol 122(6):311-317, 2000.
15. Warner MA, Saletel RA, Schroeder DR, et al: Outcomes of anesthesia andsurgery in people 100 years of age and older. J Am Geriatr Soc 46(8):988-993,1998.
16. Irvin TT: Prognosis of colorectal cancer in the elderly. Br J Surg75:419-421, 1988.
17. Mulcahy HE, Patchett SE, Daly L, et al: Prognosis of elderly patientswith large bowel cancer. Br J Surg 81:736-738, 1994.
18. Vivi AA, Lopes A, Cavalcanti SDF, et al: Surgical treatment of colon andrectum adenocarcinoma in elderly patients. J Surg Oncol 51:203-206, 1992.
19. Boyd JB, Bradford B, Watne AL: Operative risk factors of colon resectionin the elderly. Ann Surg 192:743-746, 1980.
20. Hessman O, Bergkvist L, Strom S: Colorectal cancer in patients over 75years of age-determinants of outcome. Eur J Surg Oncol 223:13-19, 1999.
21. Hesterberg R, Schmidt WU, Ohmann C, et al: Risk of elective colorectalcarcinoma in the elderly. Dig Surg 8:22-27, 1991.
22. Poon RTP, Law WL, Chu KW, et al: Emergency resection and primaryanastomosis for left-sided obstructing colorectal carcinoma in the elderly. Br JSurg 85:1539-1542, 1998.
23. Boyd JB, Bradford B, Watne AL: Operative risk factors of colon resectionin the elderly. Ann Surg 192:743-746, 1980.
24. Greenburg AG, Saik RP, Pridham D: Influence of age on mortality of colonsurgery. Am J Surg 150:65-70, 1985.
25. Irvin TT: Prognosis of colorectal cancer in the elderly. Br J Surg75:419-421, 1988.
26. Mulcahy HE, Patchett SE, Daly L, et al: Prognosis of elderly patientswith large bowel cancer. Br J Surg 81:736-738, 1994.
27. Spivak H, Maele DV, Friedman I, et al: Colorectal surgery inoctogenarians. J Am Coll Surg 183:46-50, 1996.
28. Puig-La Calle J, Quayle J, Thaler HT, et al: Favorable short-term andlong-term outcome after elective radical rectal cancer resection in patients 75years of age or older. Dis Colon Rectum 43(12):1704-1709, 2000.
29. Gardner B, Dotan J, Shaikh L, et al: The influence of age upon thesurvival of adult patients with carcinoma of the colon. Surg Gynecol Obstet153:366-368, 1981.
30. Hobler KE: Colon surgery for cancer in the very elderly: Cost and 3-yearsurvival. Ann Surg 203:129-131, 1986.
31. Kingston RD, Jeacock J, Walsh S, et al: The outcome of surgery forcolorectal cancer in the elderly: A 12-year review from the Trafford Database.Eur J Surg Oncol 21:514-516, 1995.
32. Scheele J, Stangl R, Altendorf-Hofmann A, et al: Indicators of prognosisafter hepatic resection for colorectal liver metastases. World J Surg 19:59-71,1995.
33. Fong Y, Brennan MF, Cohen AM, et al: Liver resection for colorectalmetastases. J Clin Oncol 15:938-946, 1997.
34. Fortner JG, Lincer RM: Hepatic resection in the elderly. Ann Surg211:141-145, 1990.
35. Niederhuber JE, Brennan MF, Manck HR: The National Cancer Data Basereport on pancreatic cancer. Cancer 76:1671-1677, 1995.
36. Cameron JL, Pitt HA, Yeo CJ, et al: One hundred and forty-fiveconsecutive pancreaticoduodenectomies without mortality. Ann Surg 217:430-438,1993.
37. Al-Sharaf K, Andren-Sandberg A, Ihse I: Subtotal pancreatectomy forcancer can be safe in the elderly. Eur J Surg 165(3):230-235, 1999.
38. Bottger TC, Engelmann R, Junginger T: Is age a risk factor for majorpancreatic surgery? An analysis of 300 resections. Hepatogastroenterology46(28):2589-2598, 1999.
39. Sohn TA, Yeo CJ, Cameron JL, et al: Should pancreaticoduodenectomy beperformed in octogenarians? J Gastrointest Surg 2(3):207-216, 1998.
40. Wanebo HJ, Kennedy BJ, Chmiel J, et al: Cancer of the stomach: A patientcare study by the American College of Surgeons. Ann Surg 218:583-592, 1993.
41. Bittner R, Butters M, Ulrich M, et al: Total gastrectomy: Updatedoperative mortality and long-term survival with particular reference to patientsolder than 70 years of age. Ann Surg 224:37-42, 1996.
42. Bonenkamp JJ, Songun I, Hermans J, et al: Randomised comparison ormorbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients.Lancet 345:745-748, 1995.
43. Pacelli F, Bellantone R, Doglietto GB, et al: Risk factors in relation topostoperative complication and mortality after total gastrectomy in agedpatients. Am Surg 57:341-345, 1991.
44. Viste A, Haugstvedt T, Eide GE, et al: The Norwegian Stomach Cancer TrialMembers. Postoperative complications and mortality after surgery for gastriccancer. Ann Surg 207:7-13, 1988.
45. Bandoh T, Isoyama T, Toyoshima H: Total gastrectomy for gastric cancer inthe elderly. Surgery 109:136-142, 1991.
46. Ballinger AB, McHugh M, Catnach SM, et al: Symptom relief and quality oflife after stenting for malignant bile duct obstruction. Gut 35:467-470, 1994.
47. Luman W, Cull A, Palmer KR: Quality of life in patients stented formalignant biliary obstruction. Eur J Gastroenterol Hepatol 9:481-484, 1997.
48. Dohmoto M, Hunerbein M, Schlag PM: Palliative endoscopic therapy ofrectal cancer. Eur J Cancer 32A:25-29, 1996.
49. Lopera JE, Ferral H, Whole M, et al: Treatment of colonic obstructionswith metallic stents: Indications, technique, and complications. Am J Roentgenol169:1285-1290, 1997.