Surgery Relieves Facial Paralysis due to Tumors
SAN FRANCISCO-A new surgical method for reversing facial paralysis in brain tumor patients (see photo) will be reported at the Ninth International Facial Nerve Symposium taking place July 29 to August 1.
SAN FRANCISCOA new surgical method for reversing facial paralysis in brain tumor patients (see photo) will be reported at the Ninth International Facial Nerve Symposium taking place July 29 to August 1.
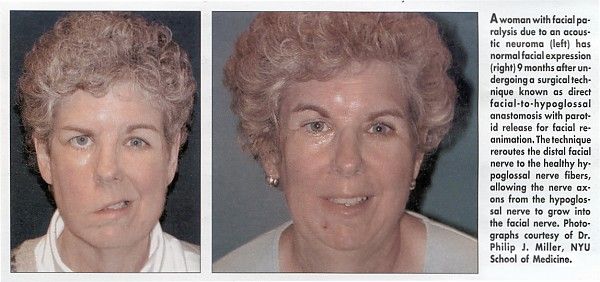
Philip J. Miller, MD, and J. Thomas Roland, MD, of New York University School of Medicine, modified an older procedure in which the distal facial nerve is rerouted to the healthy hypoglossal nerve fibers. This allows the nerve axons from the hypoglossal nerve to grow into the facial nerve.
The procedure has restored facial expression in 6 patients treated during the last 18 months at New York University Hospital, Dr. Miller said. "The more we do it, the more excited we’re getting," he told ONI in an interview. It takes 9 months for new nerve fibers to grow and animate the facial nerve before a procedure can be deemed successful, he said.
Most of the patients had acoustic neuromas or meningiomas. Dr. Miller said that the procedure, called direct facial-to-hypoglossal anastomosis with parotid release for facial reanimation, could be used in response to any condition or treatment that leaves a "structurally intact but electrically bad facial nerve."
Although technically complex, the new procedure is safe and offers advantages over jump grafts in which portions of nerves near the leg or ear are used to connect the facial nerve to the hypoglossal nerve, Dr. Miller said. With only one nerve connection instead of two, it reduces the risk of failure.
In addition, it does not introduce any sensory deficits from the harvesting of nerve grafts elsewhere in the body. "We’re not creating any new problems," he said, noting that an early technique, no longer used, completely sacrificed control over the tongue and activities such as eating in order to regain facial expression.
Dr. Miller said that the first part of the new procedure is performed by Dr. Roland, a neuro-otologist and skull-base surgeon. Dr. Roland peels the facial nerve from the bone, releasing it as close to the brain as possible. As a result, the facial nerve is almost long enough to reach the hypoglossal nerve.
Normally, the facial nerve enters the parotid gland where it exits the skeleton. Dr. Roland slices the parotid gland in half so that it dips down far enough for the facial nerve to reach the hypoglossal nerve, which is then partially severed. Some, but not all, of the hypoglossal nerve’s fibers are then spliced to the facial nerve.
No function is lost in the tongue, Dr. Miller said. "More than 50% of fibers in the hypoglossal nerve continue to provide function to the tongue, and that’s more than enough," he said. He added one caveat: "You don’t want to create a splice in the hypoglossal nerve where nerve fibers going to the tongue and neck are together. Even though the wedge takes less than 50% of the hypoglossal nerve, you could theoretically be cutting out 90% of nerve fibers going to the tongue."
The procedure averages about 3 hours, but can be done more quickly if combined with cancer surgery that exposes the bone. The patient could spend substantially more time on the operating table, however, depending on how much additional facial work is done by Dr. Miller, who specializes in facial plastic and reconstructive surgery.
Gold Weights on Eyelid
For example, he usually adds gold weights to the upper eyelid, so that the patient can close it while waiting for the nerve fibers to re-grow. This is done, Dr. Miller said, to prevent complications such as dry eye syndrome, corneal ulcers, and blindness.
To date, the new method has resulted in "a high degree of patient satisfaction, facial tone, mobility, and protection in all cases," Dr. Miller said. "We will continue to find out exactly how far we can take this. How long after the injury can this still work?"