Tamoxifen Shows Significant Reduction in Overall Recurrence in Breast Cancer
Analysis of NRG/RTOG 9804 and E5194 trials found tamoxifen significantly reduced invasive ipsilateral breast recurrence in patients with “good risk” DCIS treated without RT.
Analysis of NRG/RTOG 9804 and E5194 trials found tamoxifen significantly reduced invasive ipsilateral breast recurrence in patients with “good risk” DCIS treated without RT.
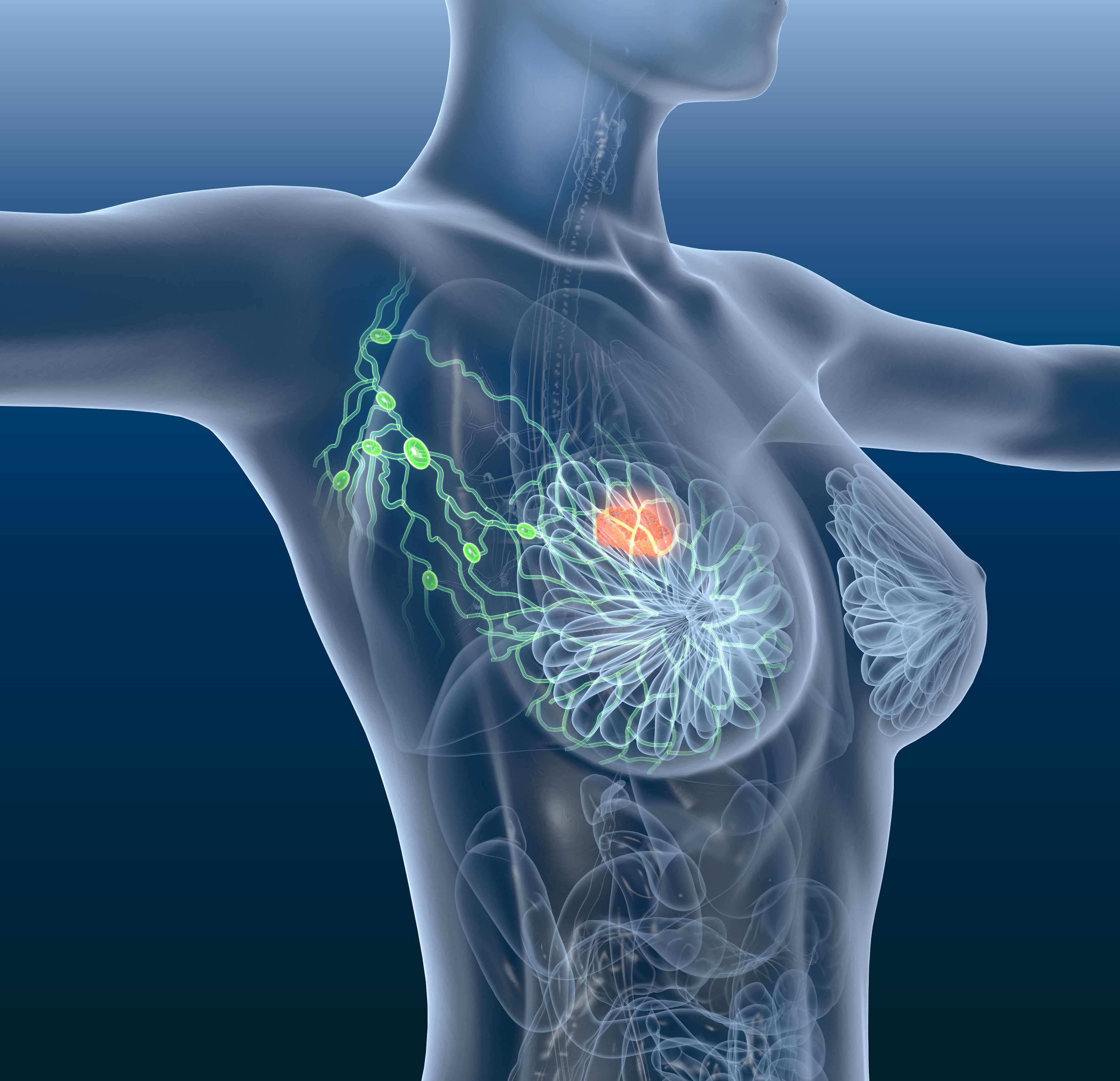
Treatment with tamoxifen (Soltamox) displayed a significant reduction in 15-year overall ipsilateral breast recurrence (IBR) in a population of patients with “good risk” ductal carcinoma in situ (DCIS) treated without radiation therapy (RT), according to findings from an ancillary analysis of the phase 3 NRG/RTOG 9804 (NCT00003857) and ECOG-ACRIN E5194 (NCT00002934) trials presented at the 2024 San Antonio Breast Cancer Symposium (SABCS).
Investigators found that treatment with tamoxifen elicited a statistically significant reduction in 15-year overall IBR by 11.4% (95% CI, 7.9%-15.5%) with tamoxifen vs 19.0% (95% CI, 15.3%-22.9%) without it (HR, 0.52; 95% CI, 0.35-0.77; P = .001). The 15-year risk of DCIS IBR was not significantly impacted by tamoxifen (5.5%) compared with those who did not receive it (8.1%; HR, 0.61; 95% CI, 0.34-1.08). For those with invasive IBR, there was a significant reduction with tamoxifen use (6.0%) compared with those who did not (11.5%; HR, 0.47; 95% CI, 0.27-0.80; P = .005). A non-significant reduction was also observed with contralateral breast events (CBE; 8.1%; HR, 0.61; 0.34-1.08; P = .09).
“Tamoxifen reduced the HR––or trended toward reducing the HR––across all subsets of patients, suggesting a broad benefit in the patients included in this analysis,” Jean Wright, MD, professor and chair of Radiation Oncology at the University of North Carolina, said in an oral presentation at SABCS. “We now have more thorough data to present to patients who are considering radiation therapy with respect to their endocrine therapy decision... Our data shows that it is important to evaluate the impact of endocrine therapy [for patients] who do not receive radiation therapy.”
Patients in the ancillary analysis of the NRG/RTOG and ECOG-ACRIN E5194 trials were included if they were considered to have “good risk” DCIS after breast-conserving surgery (BCS). “Good risk” was defined as a DCIS size of 2.5 cm or smaller, grade 1 or 2, and a margin greater than or equal to 3 mm. The use of tamoxifen was tracked in both trials, with both assessing tamoxifen alone on IBR in patients defined as “good risk” not receiving radiation therapy.
In the combined treatment analysis, 878 patients with “good risk” DCIS were included, 378 (43%) of whom received tamoxifen. Across both trials, the median age was 59 years (range, 28-88), with 80% of patients 50 years or older. Furthermore, 89% of patients were White.
Most patients had a DCIS margin width between 3 and 9 mm (n = 534, 61%) whereas only 19% had a margin width of 10 mm or greater (n = 169, 19%; P = .0001). Additionally, 48% (n = 421) of patients had a pathologic size of 5 mm or smaller vs 35% (n = 310) between 6 and 10 mm, and 17% (n = 145) had a pathologic size greater than 10 mm (P = .0001).
Furthermore, most patients had DCIS nuclear grade 2 (n = 496, 56%), with a subset of patients initially classified as low or intermediate grade upgraded to grade 3 (n = 110, 13%) after subsequent pathology review was conducted in the ECOG-ACRIN E5194 study (P = .0034).
Subgroup analysis revealed a notably high benefit in patients with a margin width of 10 mm or greater, at an IBR of 5.4% (95% CI, 1.3%-14.1%) with tamoxifen vs 24.3% (95% CI, 15.0%-34.8%) without. Furthermore, patients with a pathologic size greater than 10 mm saw a notable benefit with tamoxifen, with an IBR of 14.4% (95% CI, 5.0%-28.4%) with the agent vs 29.7% (95% CI, 19.8%-40.2%) without it.
Reference
Wright JL. Impact of tamoxifen only after breast conservation surgery for “good risk” duct carcinoma in situ: results from the NRG oncology/RTOG 9804 and ECOG-ACRIN E5194 trials. Presented at: San Antonio Breast Cancer Symposium 2024; December 10-13, 2024; San Antonio, TX. Session GS2-02