Targeted Focal Therapy: A Minimally Invasive Ablation Technique for Early Prostate Cancer
The morbidities associated with prostate cancer treatments have improved over the years. However, potential overtreatment and the risks of adverse events associated with radical treatment still pose a considerable challenge. Targeted focal therapy (TFT) of prostate cancer appears to be part of a logical continuum in the quest to improve upon the management of early organ-confined disease. TFT is a procedure in which only the cancer in the gland is ablated. The normal gland, sphincter, and in most cases the neurovascular bundles are preserved. Therefore, this approach averts some of the common complications of more radical therapy. Initial experience has been encouraging; however, long-term data and full implementation of emerging advances in imaging are urgently needed before the widespread adoption of this approach. In this review, we present the current status of our knowledge about this procedure and the most important challenges that need to be addressed. We also present the initial results with this approach at our center.
The morbidities associated with prostate cancer treatments have improved over the years. However, potential overtreatment and the risks of adverse events associated with radical treatment still pose a considerable challenge. Targeted focal therapy (TFT) of prostate cancer appears to be part of a logical continuum in the quest to improve upon the management of early organ-confined disease. TFT is a procedure in which only the cancer in the gland is ablated. The normal gland, sphincter, and in most cases the neurovascular bundles are preserved. Therefore, this approach averts some of the common complications of more radical therapy. Initial experience has been encouraging; however, long-term data and full implementation of emerging advances in imaging are urgently needed before the widespread adoption of this approach. In this review, we present the current status of our knowledge about this procedure and the most important challenges that need to be addressed. We also present the initial results with this approach at our center.
Prostate cancer is the most commonly diagnosed noncutaneous cancer in men, and the third most frequent cause of cancer mortality.[1] Treatment choice is largely dependent on clinical stage, grade, and patient preference. The treatment spectrum includes watchful waiting, active surveillance (treatment delayed until signs of progression based on serum prostate-specific antigen [PSA] and follow-up biopsies), and major therapies such as radical prostatectomy, complete cryotherapy, and various forms of radiation therapy.[2] Radical treatment has the potential to lead to urinary incontinence, impotence, and other complications. All the aforementioned treatment modalities lack the fundamental balance of achieving adequate control of the disease without compromising patient quality of life.[3]
The increasing popularity of prostate cancer screening using PSA and digital rectal exam (DRE) has raised valid concerns for overdiagnosis of clinically insignificant disease and overtreatment of many patients. A recent review of 24,405 men with low-risk prostate cancer showed that 2,564 men (10%) were overtreated with radical surgery and 10,973 men (45%) with radiation therapy.[4] The observed stage-shifting of the disease to early organ-confined, low-grade disease, underscores the concern about overtreatment of some men.
A rational alternative treatment is targeted focal therapy (TFT) of prostate cancer. This refers to the complete ablation of all clinically significant cancer foci within the prostate using a minimally invasive technique. A comparative analogy can be drawn with the evolved management of breast cancer in women, where radical mastectomy and total axillary clearance was the main treatment option until a decade ago. This was associated with significant morbidity and a prolonged postoperative recovery period. Currently, simple lumpectomy and wide excision with axillary sampling became the treatment of choice for the majority of women diagnosed with early-stage disease. This landmark shift in management has proven to be associated with a substantial improvement in morbidity incidence without compromise of a survival benefit.
Nonetheless, apparent anatomic and natural history distinctions between breast and prostate cancer must be taken into account when addressing the adoption of TFT in prostate cancer. Aside from obvious topographic differences between the two organs for utilization of imaging techniques, the challenge in the application of TFT in prostate cancer is mainly related to the fact that it is a slow-growing cancer, more often a multi-focal disease, and with bilateral involvement in more than two-thirds of newly diagnosed cases.[5] In addition, controversy surrounds the accurate depiction of clinically relevant disease as opposed to insignificant tumor burden.
Radical Treatment of the Prostate vs Active Surveillance
Appropriate management options for men with clinically localized prostate cancer remain uncertain despite increasing efforts in the past decade to introduce new techniques such as laparoscopic and robotic surgery, and conformal and hypofractionated radiotherapy. This is partly due to the lack of accurate clinical staging at the time of diagnosis and to the inability to avoid adequately damage to vital structures in the vicinity of the prostate.
The definition of clinically significant disease includes a combination of the aggregate and index (largest) tumor volume (> 5 mm3),[6] tumor grade sum (≥ 7), individual life expectancy, and cancer doubling time.[7] However, many of these parameters are difficult to define preoperatively and constitute a challenge for patient selection toward expectant management and immediate radical treatment. Accurate staging of the disease at the time of diagnosis may spare many men the adverse events experienced after any of the radical treatment modalities, when it has no survival benefit.
Large published series have revealed a significant rate of undergrading in men who underwent radical prostatectomy, as compared to the diagnostic transrectal ultrasound (TRUS)-guided biopsy Gleason score.[5] Undergrading would have, at least hypothetically, caused a missed opportunity for a more aggressive neoadjuvant combined treatment, including participation in multiple ongoing experimental clinical trials.[8] In a recently published large study depicting outcome after radical surgery for unilateral disease, clinical overstaging (pT2) occurred in about one in four patients.[9] Clearly, many patients would have missed the opportunity for a more informed decision before embarking on one of the available management options aimed at maximizing survival benefit while preserving a good quality of life.
Imaging of the Prostate
A crucial element for the future success of TFT involves advances in imaging of the prostate. Current imaging technology does not allow accurate demarcation of cancer foci within the prostate. Indeed, existing imaging modalities lack the specificity and sensitivity to aid in the early clinical staging of the disease.
Independently, computed tomography (CT) scan and even magnetic resonance imaging (MRI) with endorectal coils provide inadequate information about prostate cancer stage. However, promising advances in positron-emission tomography (PET) combined with CT provide functional and morphologic data simultaneously, improving the precise localization of the regions of uptake within the prostate. Nevertheless, limitations of the existing radioisotope fluorine-18 deoxyglucose (18F-FDG) have dampened the initial optimism for this imaging modality in identifying prostate cancer.[10]
Another emerging MRI combined imaging technique is magnetic resonance spectroscopic imaging (MRSI), a noninvasive method of evaluating metabolic markers of prostate cancer such as choline and citrate.[11] However, initial application in early-stage prostate cancer did not show a significant advantage over the use of MRI alone in this setting.[12]
Ideal imaging modalities, or a combination thereof, should be:
(1) Highly disease-specific with acceptable sensitivity for identifying prostate cancer foci
(2) Able to localize prostate cancer foci in a reproducible fashion-ie, having a real-time component for regeneration of the coordinates of tumor foci by generating a four-dimensional (4D) image
(3) Easy to use, with minimal risk to the patient
(4) Cost-effective when implemented on a large scale.
TRUS is currently the most commonly utilized imaging modality to guide prostatic biopsy and minimally invasive therapeutic options. Several modifications to the ultrasonic image, such as the use of elastography[13] and color Doppler, have not as yet produced a significant rise in accuracy for detecting and localizing prostate cancer foci. The foremost advances in ultrasound over the past decade have been focused on the rendering and segmentation of the ultrasonic image into a three-dimensional (3D) representation of the prostate.
Role of Systematic Mapping Biopsy of the Prostate
Currently, prostate biopsy is the standard of care for the initial diagnosis of prostate cancer in men presenting with significant PSA changes and/or a suspicious DRE. However, as many as 60% to 80% of the performed TRUS-guided biopsies are negative if PSA is between 2.4 and 4 ng/dL.[14] Over the past several years, emerging new data have attested to the importance of performing at least six core biopsies on each side of the prostate (extended biopsy).[15] There has been a clear departure from the historical sextant biopsy practiced. Theoretically, an increase in biopsy cores per gram volume of the prostate should yield a higher accuracy in estimating the tumor volume within the prostate, which aids in distinguishing clinical significance.[16-19] Men contemplating treatment options including active surveillance could make more informed decisions if they were presented with a more accurate description of both the extent of cancer and the Gleason grade.[20]
Commonly observed side effects of prostatic biopsy include discomfort, protracted hematuria, hematospermia, sepsis, and exacerbation of existing lower urinary tract obstructive symptoms and retention. However the majority of these side effects are self-limiting. Several studies have failed to report a significant difference in the complication rate between transrectal and transperineal approaches.[21,22] An increase in the number of biopsy cores from the prostate, theoretically, may be associated with an increased risk of adverse effects. Nonetheless, systematic mapping biopsies have been performed with adverse event rates comparable to those associated with extended biopsy. Published large series report a higher yield of detection and can be performed in the office setting with minimal sedation.[18,21]
There are two approaches to systematic biopsies-the transrectal and transperineal routes.[23] The most common clinical indication for recommending transperineal saturation biopsy is the finding of multiple negative TRUS biopsies with persistent high-risk parameters, such as rapid PSA doubling times and/or DRE abnormality. Transperineal biopsy aided by a grid has the advantage of uniform sampling of the whole prostate and better sampling of the transitional zone.[24] Moreover, this approach provides the added benefit of mapping the prostate by providing approximate coordinates of prostate cores.
Barzell and Whitmore were among the first authors to describe the transperineal approach to performing a systematic mapping biopsy of the gland (Figure 1).[25] This technique refers to an extensive prostate-size-based biopsy systematically performed using a perineal grid or a virtual real-time transrectal grid. At our institution, we adopted mapping biopsy using a transperineal approach as the preferred method for identifying patients who will potentially benefit from TFT of the prostate.
Technique for Performing Systematic Mapping Biopsies
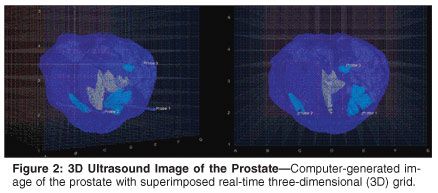
As already discussed, the localization of the specific intraprostatic cancer foci by an imaging modality or a combination of modalities is in its early stages, in terms of both the technology and the clinical validation process. Additionally, the costs associated with multiple imaging techniques represent a challenge. In the interim, ultrasound-guided systematic transperineal mapping biopsy (TRUS-MB) of the prostate using a superimposed 3D grid in real time, in our opinion, may be the only available tool to achieve a relatively accurate localization of cancer foci (Figure 2).
From our experience, several practical issues are worth noting in regard to performing a mapping biopsy of the prostate. We have studied the biopsy coordinates necessary to detect all clinically significant cancers. The use of 5-mm grid spacing when obtaining a mapping biopsy appears to be valid for detecting a higher percentage of clinically significant cancers based on our experience with a computer-simulated study of radical prostatectomy and cadaveric specimens (Table 1).[26]
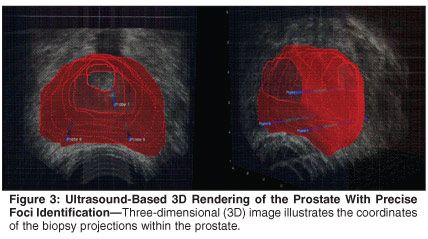
Prostate gland mobility and respiratory oscillations within the pelvis during the in vivo procedure may have a profound effect on this accuracy. We have adopted a stabilizing needle approach (used extensively in brachytherapy protocols) and artificial marking with mock beads (fiduciary markers) to overcome this hurdle (Figure 3). We believe that real-time-guided 3D imaging (4D) would be the ultimate solution by which to increase the accuracy of tumor foci localization.
Large prostates (> 60 g) may constitute another challenge. In many men with such large prostates, the pubic arch may theoretically prevent adequate transperineal access to areas of the prostate, hindering the concept of complete mapping. We believe that a combination approach (transrectal and transperineal) may have the potential to overcome this problem when a size-reduction regimen (including, for example, a 5-alpha-reductase inhibitor[27] or hormonal manipulation) has failed prior to the procedure.
Minimally Invasive Treatment of Prostate Cancer
Once the cancer is adequately mapped in the prostate, a number of ablative modalities can be utilized. As mentioned earlier, a crucial component for the success of TFT is the implementation of a safe and accurate minimally invasive treatment modality. Cryotherapy of the prostate has had a turbulent history since its early use for prostate cancer ablation. More contemporary cryotechnology and the adoption of better monitoring and warming devices have resulted in fewer complications and improvements in relapse rates. Although long-term survival data in this setting are not mature, biochemical control rates appear to be equal to other accepted modalities.
Brachytherapy, or targeted seed implantation, is another possible minimally invasive treatment for early confined prostate cancer. Other promising minimally invasive treatment modalities are emerging that could potentially provide safe and efficacious alteratives, including high-intensity focused ultrasound therapy (HIFU)[28] and photodynamic therapy (PDT).[29] HIFU, with the advantages of being minimally invasive and applicable as an outpatient procedure, appears to be the most promising. However, its focused application potential is at best unknown and requires further testing.
Patient Selection for TFT
Patients diagnosed with early organ-confined (up to stage T2b) prostate cancer with foci of cancer amenable to ablation are potential candidates for TFT. In our opinion, tumor volume burden calculated from the mapping biopsies and Gleason score should be the main criteria for patient inclusion To maximize benefit, the approximation of cancer foci to the urethra and neurovascular bundle may be viewed as relative contraindications to offering TFT. Also, men with severe lower urinary tract symptoms due to coexisting benign prostatic hyperplasia may not be ideal candidates. We suggest that aggressive medical treatment with alpha-blockers and a 5-alpha-reductase inhibitor be initiated before embarking on a targeted therapy protocol, to minimize complications such as urinary retention.
In addition to any multifocality of the primary, the controversial incidence of field-change phenomenon in the prostate is of concern. Before beginning a trial of TFT, we felt it necessary to establish that our biopsy technique was capable of identifying all components of significant cancers. In fact, as already discussed, 5-mm spaced perineal grid-based biopsies were capable of achieving this result. Yet the presence of less clinically significant small foci that may not be detected or amenable to focal treatment may predispose these men to a later recurrence.
One possible approach would be the application of low-dose radiation to the entire gland with the intent of eradicating these foci, but it is unknown whether this strategy in a neoadjuvant setting prior to focal TFT can provide a benefit in select patients. Patient selection for this combined therapy should take into account perineural invasion, high-grade prostatic intraepithelial neoplasia (HGPIN), and Gleason scores greater than 6 in the preparatory mapping biopsy results. Another strategy would be the continuous administration of a 5-alpha-reductase inhibitor. The intent would be the prevention of new neoplastic transformation and possible reversal and or stabilization of clinically less significant foci-but like the potential use of low-dose radiation, an unproven hypothesis.
How Do We Define Outcome After TFT in Prostate Cancer?
Serial PSA remains the most reliable tool for assessing biochemical failure. PSA nadir and subsequent PSA rise can provide a guide for the decision to rebiopsy and/or retreat. We believe that the open prospect of rebiopsy and possible retreatment with TFT constitute an advantage in patient management options. However, it is vital to note that at this time it is too early to determine the actual advantage, if any, of survival benefits this treatment may confer. The option of radical prostatectomy or some form of radiation therapy appears to be an option for men failing TFT. One view of TFT is that it represents a bridge between watchful waiting/surveillance and more aggressive local therapies. Only long-term, well controlled studies can address this issue.
Early Published Experience and Ongoing Protocols for TFT
Several investigators have reported early results with targeted treatment in a proportion of men diagnosed with early organ-confined unilateral prostate cancer (hemiablation). Onik et al were the first to report on cryohemiablation of the prostate in nine patients in 2002. Seven patients maintained full potency after the procedure.[30] More recently, Bahn et al published their experience with hemiablation of unilateral prostate cancer in 31 men. They reported an excellent biochemical disease-free survival (92.8%) at a mean follow-up of 70 months, with an overall potency preservation rate of 88%.[31] Although these reports appear very encouraging regarding the impact of focal treatment on quality of life, it is too early to determine the long-term survival rate associated with this procedure.
At our center, we have embarked on an institutional review board-approved protocol and are actively recruiting men for targeted cryotherapy of the prostate based on TRUS-MB. Our protocol differs from several of the previous studies in that we target the lesions rather than perform hemiablation of the gland.
As expected, our patients' interest in the procedure is overwhelming, and most men have been interested in taking part in the trial with informed consent. Entry criteria include a Gleason sum ≤ 7, T1c stage, and serum PSA < 10 ng/dL. Initial comprehensive TRUS-MB is used to accurately establish the extent of tumor burden within the prostate and to obtain the coordinates for confirmed prostate cancer foci. The average number of positive cores is 2, and the median prostate size is 34 g. Interestingly, only about 40% to 50% of men undergoing the procedure meet the entry criteria for our protocol. Overall results have yet to be reported, but we have seen two patients whose initial 12-core biopsies showed only 5% to 10% of cores with a Gleason 6 cancer, while their TRUS-MB revealed multiple foci with Gleason 8.
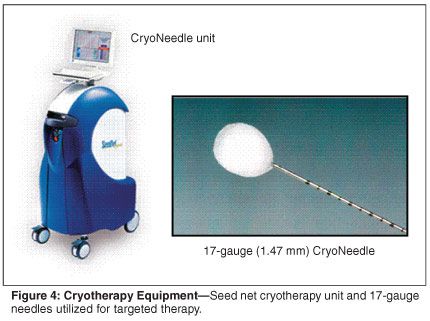
All patients with prostate volume over 50 g (with or without benign prostatic hypertrophy-related symptoms) are offered a 3-month course of a 5-alpha-reductase inhibitor prior to TRUS-MB. We utilize the 5-mm grid biopsy and have developed computer-based 3D software to segment and render a patient-specific 3D ultrasound image of the prostate (Figure 2). We find that the 3D model of the prostate and precise foci identification aids in the treatment protocol (Figure 3). TFT with cryotherapy is then utilized to ablate all foci of cancer using 17-gauge CryoNeedles (Oncura Inc, Figure 4). At an average follow-up of 3 to 6 months, no patient had any major complications. All patients have been discharged postoperatively. It is too early to comment on the results of sexual potency, although an early return appears to be the norm. No patient has reported urinary incontinence after 3 months. Longer follow-up is necessary and will be the subject of a future manuscript.
Conclusions
In summary, we believe that TFT for men with early organ-confined prostate cancer is part of a logical continuum in response to the stage shifting of the disease and the growing demand by patients for treatment alternatives that provide a better quality of life without compromising efficacy and long-term survival. Advances in imaging and minimally invasive technologies harbor the key for achieving this goal. Long-term studies are needed to confirm initial encouraging results before this approach can be adopted as a clinically viable alternative to radical management options. Clearly, TFT represents a treatment that bridges the gap between watchful waiting, active surveillance, and more radical treatments. The 5-mm grid biopsy is the procedure of choice for mapping the prostate in preparation for TFT.
Critics of TFT raise a number of important issues including risks of progression, multifocality of the disease, field-change effects, financial costs of mapping biopsies, and lack of accurate imaging techniques. Additionally, the value of monitoring PSA and performing repeat biopsies in defining success is unclear. Somewhat similar concerns were raised prior to studies determining that lumpectomy could be as effective as radical mastectomy in treating breast cancer.
Disclosures:
Dr. Barqawi is sponsored by Oncura, Inc.
References:
1. Jemal A, Siegel R, Ward E, et al: Cancer statistics, 2006. CA Cancer J Clin 56:106-130, 2006.
2. Albertsen PC, Hanley JA, Fine J: 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293:2095-2101, 2005.
3. Potosky AL, Davis WW, Hoffman RM, et al: Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: The prostate cancer outcomes study. J Natl Cancer Inst 96:1358-1367, 2004.
4. Etzioni R, Penson DF, Legler JM, et al: Overdiagnosis due to prostate-specific antigen screening: Lessons from U.S. prostate cancer incidence trends. J Natl Cancer Inst 94:981-990, 2002.
5. Gregori A, Vieweg J, Dahm P, et al: Comparison of ultrasound-guided biopsies and prostatectomy specimens: Predictive accuracy of Gleason score and tumor site. Urol Int 66:66-71, 2001.
6. Stamey TA, Freiha FS, McNeal JE, et al: Localized prostate cancer. Relationship of tumor volume to clinical significance for treatment of prostate cancer. Cancer 71:933-938, 1993.
7. Dugan JA, Bostwick DG, Myers RP, et al: The definition and preoperative prediction of clinically insignificant prostate cancer. JAMA 275:288-294, 1996.
8. Febbo PG, Richie JP, George DJ, et al: Neoadjuvant docetaxel before radical prostatectomy in patients with high-risk localized prostate cancer. Clin Cancer Res 11:5233-5240, 2005.
9. Hsu CY, Joniau S, Oyen R, et al: Outcome of surgery for clinical unilateral T3a prostate cancer: A single-institution experience. Eur Urol 2006.
10. Lawrentschuk N, Davis ID, Bolton DM, et al: Positron emission tomography and molecular imaging of the prostate: An update. BJU Int 97:923-931, 2006.
11. Fricke ST, Rodriguez O, Vanmeter J, et al: In vivo magnetic resonance volumetric and spectroscopic analysis of mouse prostate cancer models. Prostate 66:708-717, 2006.
12. Wetter A, Engl TA, Nadjmabadi D, et al: Combined MRI and MR spectroscopy of the prostate before radical prostatectomy. AJR Am J Roentgenol 187:724-730, 2006.
13. Konig K, Scheipers U, Pesavento A, et al: Initial experiences with real-time elastography guided biopsies of the prostate. J Urol 174:115-117, 2005.
14. Eggener SE, Roehl KA, Catalona WJ: Predictors of subsequent prostate cancer in men with a prostate specific antigen of 2.6 to 4.0 ng/ml and an initially negative biopsy. J Urol 174:500-504, 2005.
15. Naya Y, Ochiai A, Troncoso P, et al: A comparison of extended biopsy and sextant biopsy schemes for predicting the pathological stage of prostate cancer. J Urol 171:2203-2208, 2004.
16. Allan RW, Sanderson H, Epstein JI: Correlation of minute (0.5 MM or less) focus of prostate adenocarcinoma on needle biopsy with radical prostatectomy specimen: Role of prostate specific antigen density. J Urol 170:370-372, 2003.
17. Chan TY, Chan DY, Stutzman KL, et al: Does increased needle biopsy sampling of the prostate detect a higher number of potentially insignificant tumors? J Urol 166:2181-2184, 2001.
18. Mariappan P, Chong WL, Sundram M, et al: Increasing prostate biopsy cores based on volume vs the sextant biopsy: A prospective randomized controlled clinical study on cancer detection rates and morbidity. BJU Int 94:307-310, 2004.
19. Walz J, Graefen M, Chun FK, et al: High incidence of prostate cancer detected by saturation biopsy after previous negative biopsy series. Eur Urol 50:498-505, 2006.
20. Denberg TD, Melhado TV, Steiner JF: Patient treatment preferences in localized prostate carcinoma: The influence of emotion, misconception, and anecdote. Cancer 107:620-630, 2006.
21. Rabets JC, Jones JS, Patel A, et al: Prostate cancer detection with office based saturation biopsy in a repeat biopsy population. J Urol 172:94-97, 2004.
22. Miller J, Perumalla C, Heap G: Complications of transrectal versus transperineal prostate biopsy. ANZ J Surg 75:48-50, 2005.
23. Kawakami S, Hyochi N, Yonese J, et al: Three-dimensional combination of transrectal and transperineal biopsies for efficient detection of stage T1c prostate cancer. Int J Clin Oncol 11:127-132, 2006.
24. Pinkstaff DM, Igel TC, Petrou SP, et al: Systematic transperineal ultrasound-guided template biopsy of the prostate: Three-year experience. Urology 65:735-739, 2005.
25. Barzell WE, Whitmore WF III: How to perform transperineal saturation prostate biopsy. Urology Times. Available at www.urologytimes.com/urologytimes/article/articleDetail.jsp?id=56612. Accessed Jan 9, 2007.
26. Crawford ED, Wilson SS, Torkko KC, et al: Clinical staging of prostate cancer: A computer-simulated study of transperineal prostate biopsy. BJU Int 96:999-1004, 2005.
27. Thompson IM, Goodman PJ, Tangen CM, et al: The influence of finasteride on the development of prostate cancer. N Engl J Med 349:215-224, 2003.
28. Uchida T, Ohkusa H, Yamashita H, et al: Five years experience of transrectal high-intensity focused ultrasound using the Sonablate device in the treatment of localized prostate cancer. Int J Urol 13:228-233, 2006.
29. Moore CM, Nathan TR, Lees WR, et al: Photodynamic therapy using meso tetra hydroxy phenyl chlorin (mTHPC) in early prostate cancer. Lasers Surg Med 38:356-363, 2006.
30. Onik G, Narayan P, Vaughan D, et al: Focal "nerve-sparing" cryosurgery for treatment of primary prostate cancer: A new approach to preserving potency. Urology 60:109-114, 2002.
31. Bahn DK, Silverman P, Lee F Sr, et al: Focal prostate cryoablation: Initial results show cancer control and potency preservation. J Endourol 20:688-692, 2006.