Telemedicine Use in Oncology Practices
ABSTRACT Telemedicine (TM) will play an increasingly significant role in practices that diagnose cancers and treat patients. Although only a small percentage of oncologists currently use TM, many more will embrace this technology in the near future. Although TM has been available for several decades, it was the coronavirus disease 2019 pandemic that highlighted how useful the concept was for connecting and communicating not only with patients who live a significant distance away from their oncologist’s brick-and-mortar office, but with those who are homebound, for whatever reason. For instance, patients who have tested positive for coronavirus but who are not significantly symptomatic can be safely treated while they remain at home. One barrier to the widespread implementation of TM was lack of compensation for the time spent communicating with patients using audio-visual technology. As of March 2020, however, CMS has mandated that TM virtual visits and face-to-face visits have financial parity. This article will explore the process of implementing TM into an oncology practice with minimal time, energy, effort, and expense, as well as the concepts and the trends behind using TM to provide care for patients with cancer.
Baum is a professor of clinical urology at Tulane Medical School in New Orleans, Louisiana. He has written 8 books on practice management and the business of medicine.

Introduction
Whether they know it or not, most oncology professionals have already practiced some form of telemedicine (TM) (perhaps without the video component). TM can include taking after-hours phone calls from patients asking for medication refills, for instance. In such cases, an oncologist has the choice of calling in a refill to a pharmacy or denying the request and mandating that the patient make an appointment to receive a new prescription. The latter action, understandably, will probably not endear the oncologist to the patient, but on the other hand, providers have been aware that if they acquiesce to patients’ phone requests to have prescriptions filled—or to give medical advice by phone outside of a proscribed visit—they have been ineligible for any compensation. Now, the legal landscape and reimbursement regulations are rapidly changing, and adopting a formal TM policy may seem prudent.
Before doing so, it is important to consult with a health care attorney who understands the TM technology and state-by state regulatory and reimbursement challenges. Oncologists are held legally responsible for any advice and medications they provide to patients, even when communicating by phone or another electronic medium. It’s still true that caring for patients who intentionally call their oncologist for advice or medication refills without making or keeping appointments isn’t, overall, a sound practice: Patients may well continue to seek free medical advice if they can get away with it. However, providing care without documentation does not make for good medical practice. That’s where TM comes in—as an important adjunct to a high-functioning oncology practice. With a TM plan, oncologists can be compensated for text, phone, and video interactions with patients while practicing good medicine, as an electronic record of interactions will be generated and there will be a seamless method of billing the patient or their insurance company for the virtual visit.
Oncologists must recognize and embrace the improvements in technology that have changed the landscape of the entire health care industry—to make our practices more appealing to our patients, for one reason. Also, the proper use of TM will lower the cost of health care for both oncology patients and their providers.1 The oncology professionals who harness TM will magnify their competitive advantage exponentially as they’ll be better able to connect with existing oncology patients as well as potential new ones. Using TM, oncologists will be able to reach and attract patients in a larger geographic area, limited much less by traditionally measured distances.
Several decades ago, TM’s best use was for rural areas where there were few physicians, especially oncologists, and in that scenario, reimbursement was available.2 Now, more urban medical practices are embracing TM. A Kaiser Permanente report showed that between 2011 and 2016, telehealth service use nationally increased substantially: Growth was 629% and 960% in urban and rural areas, respectively.3
Even before the pandemic, Boston-based American Well (known also as Amwell), a TM company that connects patients with doctors over secure video, estimated that by 2022, between 341,000 and 591,000 physicians would be using telehealth to see patients.4 The American Society of Clinical Oncology has projected that between 2016 and 2026, the number of cancer survivors will rise from 15.5 million to 20.3 million.5 This increased survivorship, combined with increasing rates of new cancer in the aging population, is expected to result in a 40% increase in cancer care demand. This increase will coincide with an estimated shortage of 2200 oncologists, many of whom will be aging out of the workforce.6
Benefits of TM to oncologists
Like other health care providers, oncologists have begun to recognize the benefit of using TM in patient care. The number of physicians using TM has been increasing by about 20% per year, coinciding with growth in TM patient visits, which increased annually 261% between 2015 and 2017.7
As proposed by Berwick et al, improving the US health care system requires simultaneous pursuit of 3 aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care. This Triple Aim concept can be applied specifically to TM as well.8
Because of its efficiency, TM can reduce the expenses of caring for oncology patients. A TM program can be begun with minimal or no start-up costs. An oncologist need only have a laptop computer, smartphone, or tablet—no purchase of additional hardware or software is necessary.
TM can enhance traditional face-to-face interactions between the patient and the oncologist. A strong doctor–patient relationship almost always begins with a face-to-face encounter. While TM should not replace this traditional method of care delivery, TM can support it. With TM, providers can provide flexible, convenient care appointments for follow-up visits and check-ups, and for patient education.
For some patients, TM can be even more appealing than in-person visits. While still engaging in real-time visits, patients with busy schedules of any kind, whether due to workforce participation or providing care to children or elderly relatives, can appreciate the benefits of no travel or waiting-room time. Most patients, in fact, seek more convenient ways of accessing their health care providers and receiving immediate care.
On the provider side, more physicians than in previous decades are retiring early or experiencing burnout, because the health care profession is so challenging and stressful. Unfortunately, oncologists have one of the highest burnout rates of all physician specialties,9 and, to boot, more than 50% of practicing oncologists are aged more than 55 years and nearing retirement.10 With the aging patient population, the demand for oncology care is increasing, putting pressure on oncologists to see more patients and spend less time with each. TM can help by bridging the gap between physician supply and patient demand.11
TM can improve job satisfaction by making it easier for oncologists to interact with patients and also to balance their work and family life. This could well decrease the rate of physician burnout, which is now at an epidemic proportion, affecting 52% of all physicians.12
Cancer therapies are, of course, quite expensive, and among oncologists’ challenges are to help control health care costs. Nationally, the health care budget consumes nearly 18% of the gross domestic product, exceeding $3 trillion annually; of that, 8.6% can be attributed to physician expenses.13 Strikingly, in one report, 93% of consumers who used TM said that it lowered their health care costs.14 Lower health care costs ultimately improve the image of oncologists with our patients and the public.
Oncology patients: TM candidates
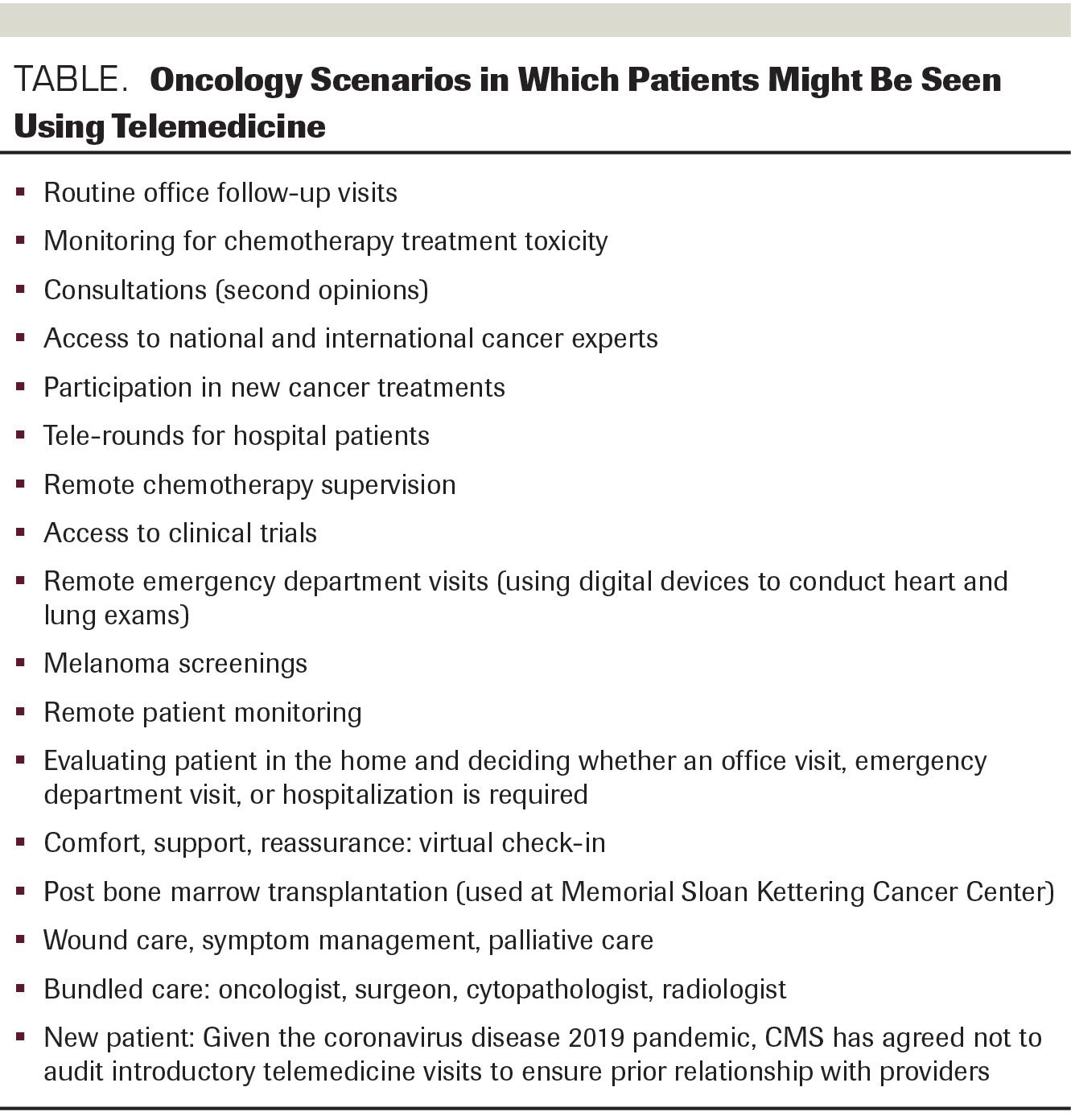
TM was first embraced by primary care physicians, dermatologists, and radiologists, and now specialists—even obstetricians and surgeons—use TM as well.15 Many of the potentially appropriate uses of TM in oncology patients are shown in the Table. Providing care for a new patient is a special case: In the past, caring for a new patient without establishing rapport, face-to-face, was not recommended. However, because of coronavirus 2019 (COVID-19), CMS has relaxed Health Insurance Portability and Accountability Act restrictions and decided that they will not audit practices and/or doctors who use TM to provide initial care.
Table. Oncology Scenarios in Which Patients Might Be Seen Using Telemedicine.
Here’s an example of an oncology patient amenable to TM management: A middle-aged, otherwise healthy woman with stage IV lung cancer was previously treated with surgery and radiation therapy and is currently receiving chemotherapy on a clinical trial protocol from Memorial Sloan Kettering Hospital. It was not convenient or prudent for the patient to travel from her Texas home to New York for a consultation and possible infusion of chemotherapy. Also, she was significantly immunocompromised, and going to her oncologist’s office would place her at risk of contracting COVID-19. Instead, she remained at home and a local physician assistant from an oncology office came to the patient’s home and conducted a virtual visit with her oncologist and surgeon in New York. Prior to the patient’s virtual visit, she was seen at home by a phlebotomist who drew and submitted the blood for the panel that was required by the trial protocol. The physician assistant performed a physical exam on the patient, including a pulmonary assessment, and reported the results to the Sloan oncologist during the TM visit. Thus the patient could remain at home and avoid COVID-19 and other communicable diseases, yet still meet with both her surgeon and oncologist. The decision was made to withhold her infusion because of an abnormal white blood-cell count and platelet count. Take-home message: For many cancer patients, having to travel a great distance every month for follow-up visits is expensive and unnecessary. Once the treatment protocol is established, many patients can be easily, safely, and effectively monitored from home.
Oncology patients: not TM candidates
In general, scenarios that are not suitable for TM involve those in which a patient has a serious/severe issue and/or those in which a physical examination, protocol-driven procedures, and aggressive interventions are or could be necessary. Other patients for whom TM is not suitable include some patients with cognitive disorders or language barriers; intoxicated patients; patients in emergency situations that warrant an office visit or a visit to the emergency department; and patients who do not have access to the technology to conduct a virtual visit.
Conclusions
TM has been available for several decades, but now the COVID-19 pandemic has changed the playing field. TM enables communication with our oncology patients when face-to-face visits or in-person examinations are not required. The moment of mass adoption of TM has arrived, and more and more patients will be requesting virtual visits with their oncologists.
FINANCIAL DISCLOSURE: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References
- Lafolia T. Research review: Does telehealth really save on costs. eVisit. Accessed June 8, 2020. https://blog.evisit.com/research-review-does-telehealth-really-save-on-costs)
- Zundel KM. Telemedicine: history, applications, and impact on librarianship. Bull Med Libr Assoc. 1996;84(1):71-79.
- Barkholz D. Kaiser Permanente chief says members are flocking to virtual visits. Modern Healthcare. April 21, 2017. Accessed June 8, 2020.http://www.modernhealthcare.com/article/20170421/NEWS/170429950?utm_source=
- Amwell. Telehealth Index: Physician Survey 2019. Accessed June 8, 2020. https://static.americanwell.com/app/uploads/2019/04/American-Well-Telehealth-Index-2019-Physician-Survey.pdf
- Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363-385. doi:10.3322/caac.21565
- AAMC updates physician shortage projections. American Hospital Association. April 25, 2019. Accessed June 8, 2020. https://www.aha.org/news/headline/2019-04-25-aamc-updates-physician-shortage-projections
- Lagasse J. Telemedicine is poised to grow as its popularity increases among physicians and patients. Healthcare finance. July 16, 2019. Accessed June 8, 2020. https://www.healthcarefinancenews.com/news/telemedicine-poised-grow-its-popularity-increases-among-physicians-and-patients
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
- Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol. 1991;9(10):1916-1920. doi:10.1200/JCO.1991.9.10.1916
- Hortobagyi GN; American Society of Clinical Oncology. A shortage of oncologists? The American Society of Clinical Oncology workforce study. J Clin Oncol. 2007;25(12):1468-1469. doi:10.1200/JCO.2007.10.9397
- Physician burnout in 2019, charted. Advisory Board. January 18, 2019. Accessed June 8, 2020. https://www.advisory.com/daily-briefing/2019/01/18/burnout-report#:~:text=More%20than%2040%25%20of%20physicians,National%20Physicians%20Burnout%20%26%20Depression%20Report.
- Shanafelt TD, Dyrbye LN, West CP. Addressing Physician Burnout: The Way Forward. JAMA. 2017;317(9):901-902. doi:10.1001/jama.2017.0076
- Physician pay accounts for 8.6% of total healthcare expenses. Hospital Review. Accessed June 8, 2020. https://www.beckershospitalreview.com/compensation-issues/physician-pay-accounts-for-86-of-total-healthcare-expenses.html
- Healthmine. The 2016 HealthMine Digital Health Report: State and Impact of Digital Health Tools. Spring/Summer 2016. Accessed June 8, 2020. http://healthmine.com/wp-content/uploads/2019/07/HealthMine_Digital_Health_Tools_Report_May_2016.pdf
- de Mooij MJM, Hodny RL, O'Neil DA, et al. OB Nest: Reimagining Low-Risk Prenatal Care. Mayo Clin Proc. 2018;93(4):458-466. doi:10.1016/j.mayocp.2018.01.022