The Proper Ways to Identify and Use ADCs in Breast Cancer Subtypes
Deciding when to use immunotherapy and how to utilize antibody-drug conjugates are complicated processes that require multidisciplinary collaboration to ensure that all patients with breast cancer receive appropriate and efficient care.
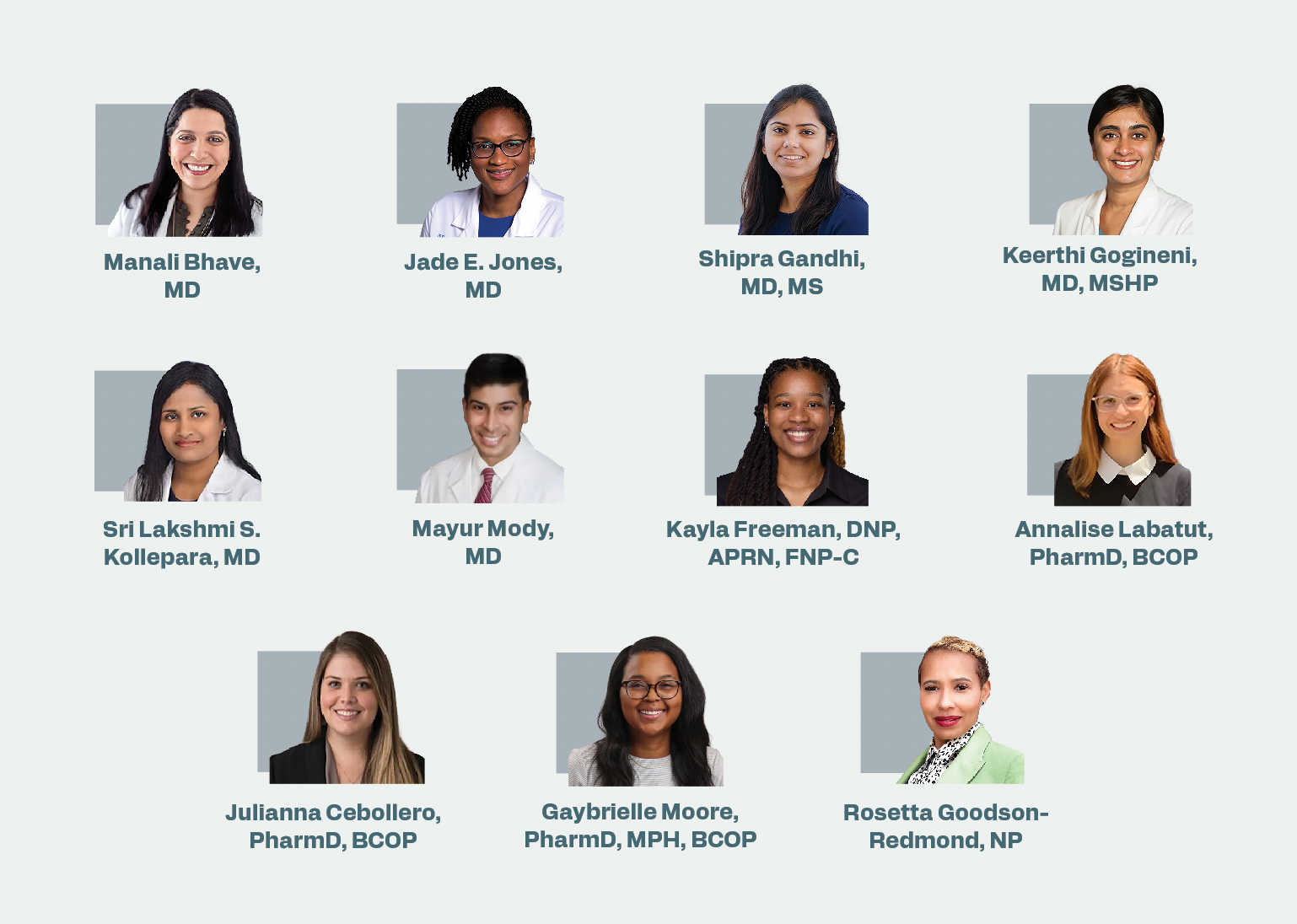
The authors
A panel of cancer care specialists, including oncologists, nurses, and pharmacists, discussed the nature of care for patients with triple-negative breast cancer and hormone receptor (HR)–positive, HER2-negative metastatic breast cancer. The discussion was part of a CancerNetwork-hosted Satellite Sessions program, and the experts touched on when they would turn to immunotherapy, particularly antibody-drug conjugates (ADCs), and how they would handle select patient cases. The ADCs of note were fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu), sacituzumab govitecan-hziy (Trodelvy), and datopotamab deruxtecan-dlnk (Dato-DXd; Datroway).
The panel was led by Manali Bhave, MD, an assistant professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine and the medical director of the Phase I Clinical Trials Unit at Winship Cancer Institute of Emory University in Atlanta, Georgia, and Jade E. Jones, MD, an assistant professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine. Fellow panelists were Shipra Gandhi, MD, MS, an associate professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine and the director of breast translational research at Glenn Family Breast Center at Winship Cancer Institute; Keerthi Gogineni, MD, MSHP, an associate professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine and the director for education of fellows and residents at Grady Health System; Sri Lakshmi S. Kollepara, MD, a clinical assistant professor at Morehouse School of Medicine in Atlanta, Georgia; Mayur Mody, MD, a hematologist-medical oncologist at Advent Health; Kayla Freeman, DNP, APRN, FNP-C, a lead advanced practice provider for breast oncology at Emory Winship Cancer Institute; Annalise Labatut, PharmD, BCOP, an oncology clinical pharmacy specialist in breast oncology for Emory Healthcare/Winship Cancer Institute; Julianna Cebollero, PharmD, BCOP, a clinical pharmacy specialist for outpatient care at Grady Health System; Gaybrielle Moore, PharmD, MPH, BCOP, a clinical pharmacy specialist in breast and gynecologic oncology at Emory Winship Cancer Institute; and Rosetta Goodson-Redmond, NP, a nurse practitioner at Winship Cancer Institute of Emory University.
Making Immunotherapy Decisions
Bhave / Beyond PD-L1 expression, what other molecular signatures or clinical factors have helped guide your immunotherapy decisions in the first-line setting for metastatic triple-negative breast cancer [TNBC]?
Gandhi / Beyond PD-L1, if the tumor mutation burden is high—we don’t have approval in the first line—I might want to treat with immunotherapy. With PD-L1 negativity, if the tumor mutation burden is high, I might consider pembrolizumab (Keytruda) with chemotherapy for that patient.
Gandhi / In the first-line setting, if I’m trying to find a reason for immunotherapy and PD-L1 is negative—I don’t think it would be very frequent that PD-L1 is negative and tumor mutation burden is high—that would be a situation when I would consider using [immunotherapy] in the first-line setting.
Bhave / Do you foresee that, even in early-stage TNBC, we will utilize [tumor-infiltrating lymphocytes (TILs)] for benefit with chemotherapy or immunotherapy in metastatic and early-stage [disease]?
Gandhi / The [phase 2 NeoTRACT trial (NCT05645380)] is studying this very question. If TILs are high, they’re treating patients with carboplatin, [docetaxel], and pembrolizumab.1 If the TILs are low, that’s when they think there may be a role for anthracyclines or more doses of chemotherapy. It’s a TIL-based regimen in triple-negative breast cancer [in] the NeoTRACT trial. There is an evolving role for using TILs as a biomarker in the early-stage setting.
Gogineni / In the early-stage setting, there are nice data in the residual disease space where we know these patients are at a super high risk of recurrence. There’s a big difference in recurrence if you stratify the residual disease burden score by TIL. If you [have] high TIL and have a residual cancer burden [RCB]-II [classification], you do better than if you have an RCB-II [classification] and have low TILs. It’s an interesting, unsurprising pattern and another way to risk-stratify which patients need more aggressive [radiation therapy].
Utilizing ADCs
Bhave / In clinical practice, how are we utilizing these ADCs [for] a patient who comes in with de novo PD-L1–negative metastatic TNBC? What is typically your frontline [therapy]? When do you consider utilizing ADCs?
Kollepara / For TNBC, even though it’s PD-L1 negative, we look for BRCA mutations and HRR mutations to see if there’s any role for [ADCs]. Otherwise, the standard of care is the combination of chemoimmunotherapy that we go with; ADCs come in after 2 lines [of therapy]. That’s how we are using them in clinical practice.
Bhave / If the patient [has] PD-L1–negative [disease], do you typically start with chemotherapy and then the ADCs?
Kollepara / Yes. The chemotherapy is what we do with patients who [have] PD-L1–negative [disease] with the regular-dose ADC or the [gemcitabine plus oxaliplatin]. Then we go for the ADC down the line.
Mody / Usually, these patients have a heavy disease burden; I’ll use cytoreductive chemotherapy first. Sometimes it’s just a singlet, sometimes it’s a doublet. I have not given immunotherapy to a [patient who has] PD-L1–negative [disease] up front. I’ve done…doublet chemotherapy and saved [the ADCs] for the second line. I’ve had about 2 cases like this so far. ADCs in the second line would be my answer.
Kollepara / I agree with Mayur saying [we do] the taxanes or the platinum-based [therapy] in the first line, but then you always think about the [patient who has] HER2-low [disease], present or not. Based on that, you can do T-DXd in that scenario.
Gogineni / If the patient isn’t [experiencing] early relapse after having had curative-intent [therapy] and they [have] PD-L1–negative [disease], sometimes just for the sake of this person getting a break, I will think about stalling with capecitabine to get them out of an infusion setting. It depends on the burden of their disease and how quickly they [experience] relapse or if they received capecitabine in a residual disease setting before.
Bhave / For patients who are progressing and who had a recurrence after [the phase 3 KEYNOTE-522 trial (NCT03036488) regimen of pembrolizumab, paclitaxel, and carboplatin], how would you consider your treatment options?2 How does that depend on the treatment-free interval or prior exposure to immunotherapy when you’re thinking about that frontline TNBC treatment?
Freeman / If they’ve had previous exposure to immunotherapy, I haven’t seen it where we’ve revisited immunotherapy later in other settings.
Jones / If a person [has] recurring [disease] within 6 months of surgery—they may be on gemcitabine or maybe have just finished gemcitabine—they don’t respond to chemotherapy, so I try to get ADCs for my patients with TNBC. Sacituzumab govitecan is often what I use first within those 6 months. Unfortunately, sometimes insurance will still want you to do another [round of] chemotherapy first, but I’ve had bad outcomes when I’ve been forced to give chemotherapy first in that setting. I’ve been more successful getting responses from patients when they are getting an ADC in that 6-month time frame.
Deciding Which ADC to Choose
Jones / How do you interpret the differences in trial designs between the [phase 3 DESTINY-Breast04 trial (NCT03734029), the phase 3 TROPiCS-02 trial (NCT03901339)], and [the phase 3 TROPION-Breast01 trial (NCT05104866)]? Does overall survival impact your treatment choice? When you’re talking about deciding between sacituzumab govitecan, Dato-DXd, or even T-DXd, do you factor in not having an overall survival benefit in the Dato-DXd arm?
Gandhi / No, because there is a reason why we are not seeing an overall survival difference. By the time [the TROPION-Breast01 trial] was designed, other ADCs were already approved. The control arm that received chemotherapy could have received ADCs after that. That’s probably the reason we are not seeing an overall survival difference here. At this time, this does not influence my selection sequencing. [My decision whether to use it] is more based on the adverse event profile.
Jones / Has anyone used Dato-DXd so far?
Labatut / My clinic in total has 4 patients on Dato-DXd right now, and the overarching theme is that we are reaching for Dato-DXd for those who do not qualify for T-DXd and cannot otherwise tolerate sacituzumab govitecan.
Jones / What is the tolerance that you’ve noticed…in terms of seeing patients complaining about some of the stomatitis?
Labatut / It’s early. So far, so good. The prophylactic dexamethasone mouth rinse is 4 times a day, as well as the preservative-free lubricant eye drops. The maintenance for the patient for their supportive care medications and for the prophylactic regimens is a lot. There’s a high, not “pill burden” per se, but both are 4 times a day, so there is a lot to keep up with.
Jones / When we’re talking about all the ADCs and the HER2-low [disease], what are the most challenging adverse effects?
Moore / The neutropenia with sacituzumab govitecan has been the one we have to be the most proactive about in terms of…planning for the use of short-acting and long-acting growth factor. One that we haven’t mentioned yet is the nausea. The emetogenic potential of T-DXd was upgraded from moderate to high emetogenicity [by the NCCN]. With our treatment plans at Winship Cancer Institute, we’ve updated those to make sure that they’re getting that up-front antiemetic 3-drug regimen, and [we’re] having to educate patients about the use of antiemetics at home and sometimes even having to add in a fourth one like olanzapine for that additional breakthrough nausea that might be occurring.
Those are the 2 biggest ones that we are often brought in to help with as far as a pharmacy team. I don’t have any experience with [Dato-DXd] quite yet, but the mucositis is something that we have to be proactive about. In addition to the [dexamethasone] rinse, we also have patients chew ice during that infusion to help prevent the mucositis.
A Sacituzumab Govitecan Patient Case
Jones / You have a 68-year-old [woman] whom [has] HR-positive, strongly estrogen receptor–positive [disease] and [has] HER2 [immunohistochemistry] 0, and her previous treatments included endocrine therapy with a CDK4/6 inhibitor, fulvestrant (Faslodex) plus a PIK3CA inhibitor, and gemcitabine. She was initiated on sacituzumab govitecan after progression, and unfortunately, at the first cycle on day 8, she experienced grade 3 neutropenia. How would you approach this?
Goodson-Redmond / At the start of the treatment plan, we would go ahead and try to get the short-acting and the long-acting growth factors [approved] for these patients so that we don’t [have] that issue. We had a little pushback recently with trying to get both, so we chose the short-acting over the long-acting [growth factor]. Of course, when this happens and we don’t have the growth factor in place, we hold until the absolute neutrophil count is at an acceptable level.
Cebollero / I agree with Rosetta. Just getting those approved up front [is important]. We need to make sure that the absolute neutrophil count is above the 1500-cells/μL cutoff. If we need to, for those patients, we may decrease the dose level if they have not recovered in a timely fashion after the growth factor.
Jones / If it happens on day 8, you are trying to get short-acting growth factor between day 2 and day 5. Is anyone changing the interval so you see it on day 1, day 8? Would anyone, instead of giving the growth factor, just do day 1, day 15?
Labatut / I do it often, especially if it happens early, going into that first cycle—that very first day 8. It possibly insinuates that they [have] UGT1A1 [deficiency] or homozygous [disease]. That’s something we test for up front. Even if they [do] not, if it’s a significant neutropenia, grade 3 or higher, I have a low threshold to suggest it.
Cebollero / We’ve also done that, especially considering the feasibility of getting an infusion appointment. If we’ve already rescheduled you once or twice or we’ve had to delay your treatment, that approach of adding the day 1, day 15 would be a good approach.
References
1. Stecklein SR, Aripoli A, Salgado S, et al. NeoTRACT: phase II trial of neoadjuvant tumor infiltrating lymphocyte- and response-adapted chemoimmunotherapy for triple-negative breast cancer (TNBC).J Clin Oncol. 2024;42(suppl 16):TPS629. doi:10.1200/JCO.2024.42.16_suppl.TPS629
2. Schmid P, Cortes J, Pusztai L, et al; KEYNOTE-522 Investigators. Pembrolizumab for early triple-negative breast cancer. N Engl J Med. 2020;382(9):810-821. doi:10.1056/NEJMoa1910549
Gedatolisib Combo With/Without Palbociclib May Be New SOC in PIK3CA Wild-Type Breast Cancer
December 21st 2025“VIKTORIA-1 is the first study to demonstrate a statistically significant and clinically meaningful improvement in PFS with PAM inhibition in patients with PIK3CA wild-type disease, all of whom received prior CDK4/6 inhibition,” said Barbara Pistilli, MD.