Thermal Imaging May Be an Adjunct to Mammography
SEATTLE-When used as an adjunct to mammography and clinical breast examinations, thermal imaging may help reduce the number of unnecessary breast biopsies, according to Karleen Callahan, PhD, director of Clinical Research for Breast Cancer at Computerized Thermal Imaging, Inc (CTI).
SEATTLEWhen used as an adjunct to mammography and clinical breast examinations, thermal imaging may help reduce the number of unnecessary breast biopsies, according to Karleen Callahan, PhD, director of Clinical Research for Breast Cancer at Computerized Thermal Imaging, Inc (CTI).
Dr. Callahan presented an exhibit about the CTI Breast Cancer System 2100 (BCS 2100), an investigational thermal imaging device, at the 101st Annual Meeting of the American Roentgen Ray Society (ARRS).
Dr. Callahan and her colleagues are analyzing the results of a 3½-year clinical study of the efficacy of the BCS 2100 as an adjunctive breast imaging modality in the diagnostic setting. In this multicenter study, thermal imaging was performed before biopsy in more than 2,100 women who had been referred for biopsy because of mammographic findings and/or palpable findings.
The findings are likely to be particularly meaningful because the patient population included women of a wide range of ages and ethnicities. "Our clinical study pretty well reflects the demographics of the country," Dr. Callahan said.
Thermal imaging provides physiologic information about suspicious areas of the breast. The physiologic basis for thermal imaging for cancer detection is the difference in infrared emissions of normal and malignant tissues upon cooling. This difference results, in turn, from differences in angiogenesis, vascular reactivity, the release of vasoactive mediators, and metabolic activity.
Efforts to harness thermal disparities for breast cancer detection date back to at least the 1970s, Dr. Callahan said. But that older technology (called thermography) had limitations and did not prove effective when used for breast cancer screening. The key changes have been an increase in the camera sensitivity, the collection of data over a period of several minutes, the addition of a cooling challenge, and the development of a sophisticated computer model for analyzing the data. "We think that all of the improvements will make thermal imaging a viable technique," she said.
A patient undergoing thermal imaging lies prone on the patented BCS 2100 imaging table, and thermal data are collected from each breast over a 3-minute period that includes a cooling challenge (a stream of cold air blown over the breast).
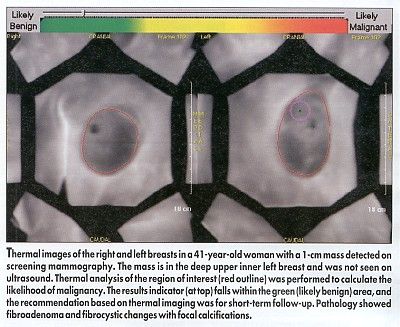
The radiologist identifies the region of interest from the mammogram or the clinical breast exam and uses this region of interest to localize the lesion on the thermal image. A proprietary algorithm analyzes unique spatial and temporal characteristics in the data to generate a likelihood of malignancy score for the lesion (see Figure).
Patient acceptance of the BCS 2100 has been very good, Dr. Callahan said. "It’s not an uncomfortable procedure. There’s no breast compression, and it’s not invasiveno contrast dyes and no radiation," she said. The entire exam takes only about 10 minutes.
Unblinding of the data from the clinical study should provide detailed information about the performance of the BCS 2100, Dr. Callahan said. For example, the data will help determine how effective the BCS 2100 is for detecting specific types of malignancies, how well it discriminates between malignant and benign neoplasms, and how well it performs for superficial vs deep lesions.
Thermal imaging may be particularly useful in women with lesions that are probably benign (BI-RADS 3) or suspicious (BI-RADS 4) on mammography, Dr. Callahan noted. "Right now, these patients often go to biopsy. And yet, about 80% of the biopsies turn out to be benign," she said. "Thermal imaging would provide further information to the doctor and the patient as to whether they might want to proceed to biopsy or possibly go to short-term follow-up."
To obtain premarket approval (PMA) of the BCS 2100, the company is using the FDA’s modular approach, which divides the application into five modules, each containing a portion of the total data required. The FDA has accepted four modules for the BCS 2100, and the final module was submitted last month.