Three-Drug Combo Improved PFS in Relapsed, Refractory Myeloma
Panobinostat added to bortezomib/dexamethasone for treating relapsed/refractory multiple myeloma improved progression-free survival and complete response rates.
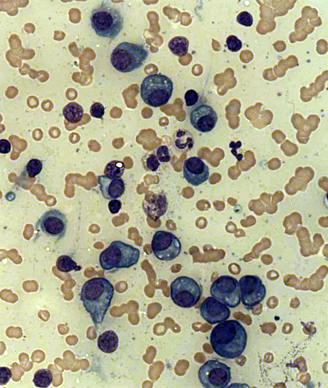
Plasma cells in a case of multiple myeloma; source: Dr. Erhabor Osaro.
The addition of panobinostat to bortezomib and dexamethasone for the treatment of relapsed or relapsed and refractory multiple myeloma resulted in an almost 4-month improvement in progression-free survival and a significant improvement in the rate of complete or near complete response, according to the results of the PANORAMA1 study.
“PANORAMA1 is the first phase III trial to show a benefit for a three-drug combination compared with a two-drug combination in patients with relapsed or relapsed and refractory multiple myeloma,” wrote JeÅus F. San-Miguel, MD, of ClÃnica Universidad de Navarra-CIMA, Spain, and colleagues. “Together with the results of PANORAMA2, which showed the efficacy of panobinostat, bortezomib, and dexamethasone in patients with bortezomib-refractory disease, these findings validate the hypothesis of deacetylase inhibition and suggest that panobinostat could be an important addition to the treatment armamentarium for patients with multiple myeloma.”
The results of PANORAMA1 were presented at the 2014 ASCO Annual Meeting and were published recently in Lancet Oncology.
PANORAMA1 included 768 patients enrolled between January 2010 and February 2012 who were randomly assigned to 21 days of panobinostat (20 mg on days 1, 3, 5, 8, 10, and 12), bortezomib (1.3 mg/m2 on days 1, 4, 8, and 11) and dexamethasone (20 mg on days 1, 2, 4, 5, 8, 9, 1, and 12) or placebo plus dexamethasone/bortezomib.
After a median follow-up of 6.47 months for the panobinostat group and 5.59 months for the placebo group, the median progression-free survival was 11.99 months for panobinostat compared with 8.08 months for placebo (HR = 0.63; 95% CI, 0.52-0.76; P < .0001).
Overall survival data are not yet mature, and overall response rate was not significantly different between the two groups. However, the data did show that a higher percentage of patients in the panobinostat group achieved complete or near complete response compared with the placebo group (27.6% vs 15.7%; P = .00006).
Severe adverse events were reported in 60% of the panobinostat group and 42% of the placebo group. Twice as many patients assigned panobinostat experienced thrombocytopenia (67% vs 31%). Other common grade 3/4 adverse events seen with panobinostat were lymphopenia (53%), diarrhea (26%), asthenia or fatigue (24%), and peripheral neuropathy (18%).
In an editorial that accompanied the results, S. Vincent Rajkumar, MD, of Mayo Clinic, Rochester, Minn., pointed out several caveats to the study, including the fact that there was no difference in overall response between the two treatment groups, that, although not yet available, quality-of-life data will likely show that use of panobinostat affects quality of life when given at the dose used in this study, and that the twice-per-week dosing of bortezomib used in this study has since been shown to have an unacceptable toxicity profile.
“I expect panobinostat to become an important component of myeloma treatment. However, it will probably be approved with a recommended dosing schedule that is not realistic,” Rajkumar wrote. “San-Miguel and colleagues’ trial emphasizes a dilemma wherein changes in standard treatment occur during the course of a study. This issue is likely to occur more often in the future as drugs come to market before we really know the right way to use them. In this case, most patients will surely be treated with lower doses of both panobinostat and bortezomib than are likely to be specified on the prescribing label.”
Novartis, the manufacturer of panobinostat, submitted an application for approval of the drug to the US Food and Drug Administration (FDA) in June. The FDA has granted the drug priority review.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.